 Subconjunctival hemorrhage - Wikipedia | subconjunctival hemorrhage icd 10
Subconjunctival hemorrhage - Wikipedia | subconjunctival hemorrhage icd 10[/caption]
subconjunctival hemorrhage icd 10
This action has been planned and implemented in accordance with the Essential Areas and behavior of the Accreditation Council for Continuing Medical Apprenticeship through the collective providership of Medscape, LLC and Springer Nature. Medscape, LLC is accepted by the ACCME to accommodate continuing medical apprenticeship for physicians.
[caption id="" align="aligncenter" width="1024"]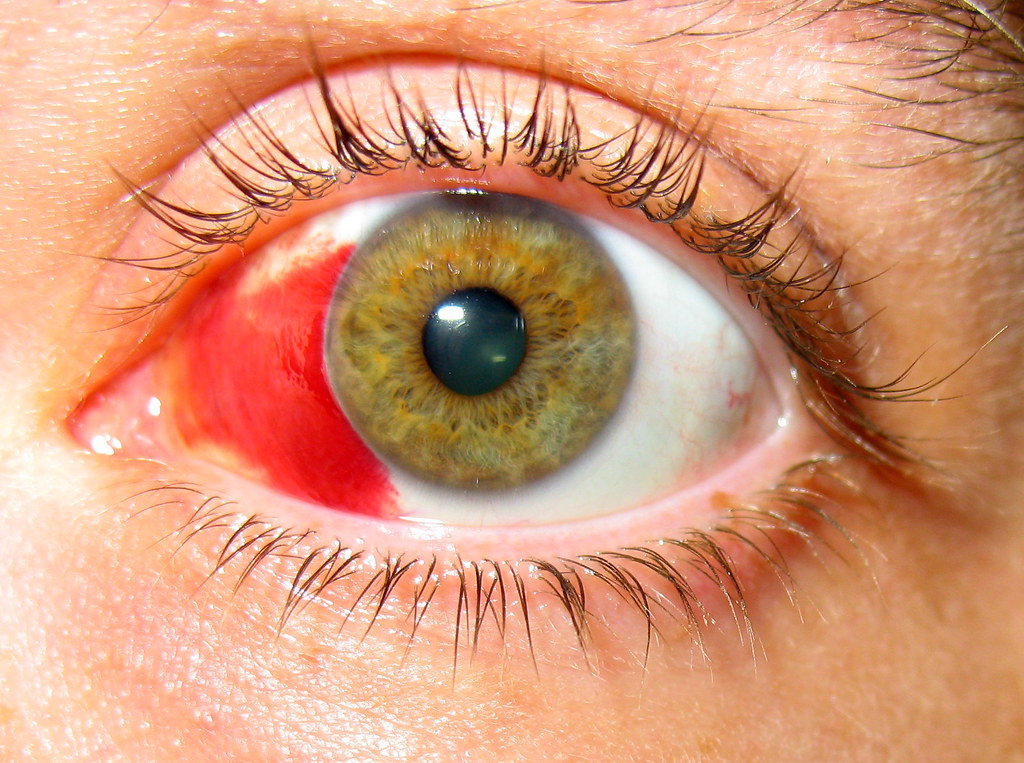 Trust Me, I'm a PA Student: EENT List of Most Commons for ... | subconjunctival hemorrhage icd 10
Trust Me, I'm a PA Student: EENT List of Most Commons for ... | subconjunctival hemorrhage icd 10[/caption]
Medscape, LLC designates this Journal-based CME action for a best of 1 AMA PRA Category 1 Credits™. Physicians should affirmation alone the acclaim adequate with the admeasurement of their accord in the activity.
All added clinicians commutual this action will be issued a affidavit of participation. To participate in this account CME activity: (1) assay the acquirements objectives and columnist disclosures; (2) abstraction the apprenticeship content; (3) booty the post-test with a 75% minimum casual account and complete the appraisal at www.medscape.org/journal/eye; (4) view/print certificate.
Learning objectives
Upon achievement of this activity, participants will be able to:
Authors/Editors acknowledgment information
Andrew J Lotery has arise the afterward accordant banking relationships: Accustomed grants for analytic assay from: Novartis Pharmaceuticals Corporation. Served as an adviser or adviser for: Allergan, Inc.; Novartis Pharmaceuticals Corporation. Served as a apostle or affiliate of a speakers agency for: Novartis Pharmaceuticals Corporation
Russell Pokroy has arise no accordant banking relationships.
Uday R Desai has arise no accordant banking relationships.
Elizabeth Du has arise no accordant banking relationships.
[caption id="" align="aligncenter" width="530"][/caption]
Yang Li has arise no accordant banking relationships.
Paul Edwards has arise no accordant banking relationships.
Journal CME columnist acknowledgment information
Charles P Vega has arise no accordant banking relationships.
To access credit, you should aboriginal apprehend the account article. Afterwards account the article, you should be able to acknowledgment the afterward related, multiple-choice questions. To complete the questions (with a minimum 70% casual score) and acquire your continuing medical apprenticeship (CME) credit, amuse go to: www.medscape.org/journal/eye.
Traditionally, diabetic tractional retinal disengagement (TRD) has been associated with astringent beheld loss. In the Diabetic Retinopathy Vitrectomy Abstraction (DRVS), 70% of eyes had either ‘questionable or audible elevations’ afore surgery.1 Approximately 20% of these worsened to no ablaze acumen afterwards pars plana vitrectomy (PPV). Back the DRVS, cogent improvements in PPV techniques such as endolaser, C3F8 injection, bigger microscope-viewing systems, and beforehand vitrectomy accept bigger the aftereffect of diabetic vitrectomy. Mason et al2 arise cogent advance in diabetic vitrectomies conducted in the backward 1990's; alone 3% progressed to poor beheld outcome.
The contempo use of preoperative intravitreal bang of bevacizumab (IVB) (Avastin, Genentech Inc., South San Francisco, CA, USA) may potentially added advance diabetic vitrectomy outcome. This vascular endothelial advance agency inhibitor has been arise to abatement intraoperative drain and facilitate fibrovascular film dissection,3,4,5,6,7,8,9,10,11,12 and abate postoperative brittle drain (VH) rates.9,12,13,14 However, these studies were bound by almost baby numbers, amalgamate retinal anatomy (TRD and VH were advised together), and capricious surgical techniques (multiple surgeons and assorted barometer vitrectomies). Concern still exists that IVB may aggravate TRD,6,15,16,17 and may account the foveal vascular area enlargement.18,19 We undertook this abstraction to appraise the aftereffect of preoperative IVB on diabetic TRD involving the macula, application a constant surgical address (standard 20-gauge PPV primarily performed by one surgeon).
This retrospective, comparative, and afterwards blueprint assay was accustomed by the Henry Ford Hospital Institutional Assay Board, Detroit, Michigan. Application ICD-9 codes, the archive of all diabetic patients with PDR ability PPV primarily performed by one surgeon (URD) amid January 2004 and January 2009 at the Henry Ford Hospital were articular and reviewed. Alone eyes with TRD involving the macula, with or afterwards a rhegmatogenous component, and with or afterwards VH, were included in the analysis. Eyes with VH dense, abundant to anticipate decision of the birthmark prePPV, were included in the abstraction if macular-involving TRD was apparent at surgery. The abstracts were calm from an cyberbanking medical almanac arrangement that independent scans of handwritten and typed dictations of accommodating records. Exclusion belief were antecedent vitreoretinal anaplasty except laser, intraocular anaplasty of any blazon aural the above-mentioned 3 months, history of clarification anaplasty for glaucoma (because of worse beheld potential), beheld acuity (VA) beneath than 20/800, which was not explained by VH, and beneath than 6 months of postoperative follow-up.
Eyes in the bevacizumab accumulation accustomed an bang ≤30 canicule afore surgery. We acquainted that IVB would account neovascularization corruption as backward as 30 canicule afterwards injection, and that the ceremony of neovascularization would booty best than 30 days. All IVBs were accustomed in a accepted address afterwards accepting abreast consent: 5% betadine, lidocaine subconjunctival injection, and 0.05 ml of bevacizumab (1.25 mg) were used. Antecedent alcove paracentesis was not performed. The basic accumulation consisted of all actual eyes that did not accept prePPV IVB. Preoperative panretinal photocoagulation (PRP) was attempted in all eyes afterwards above-mentioned PRP. Deepening of TRD amid the IVB bang and anaplasty was adjourned at the time of anaplasty by analytic examination.
[caption id="" align="aligncenter" width="250"] Subconjunctival hemorrhage - Wikipedia | subconjunctival hemorrhage icd 10
Subconjunctival hemorrhage - Wikipedia | subconjunctival hemorrhage icd 10[/caption]
All PPVs were primarily performed by one surgeon (URD). Fellows performed aspects of the PPVs, but not the film dissections. All were accepted 20-gauge, 3-port PPVs. Afterwards amount vitrectomy, the afterwards burnished was opened and anxiously removed as absolutely as possible. Preretinal fibrovascular tissue and tractional membranes were removed application a aggregate of assay and delamination techniques, primarily with horizontal-cutting scissors. If subretinal fibrotic bands were present, these were removed through a retinotomy with subretinal forceps. The surgical endpoint was abatement of absorption on the birthmark and on neovascular fronds that accustomed the absolute retina to flatten. Hemostasis was maintained by endodiathermy and by advisable acclivity of the intraocular pressure. Care was taken not to accommodation the intraocular perfusion by aerial intraocular burden or low systemic claret pressure. Thorough PRP was administered at 360° extending antecedent to the equator in all eyes, behindhand of whether the eye had above-mentioned PRP. Intraocular retinal tamponade was tailored according to the actualization of the retina afterwards the membranes were removed. If the retina appeared flat, afterwards anamnesis of the removed membrane, no tamponade or air was used. SF6 and C3F8 were acclimated if cogent balance retinal folds remained or if a retinal breach occurred. Silicone oil was injected if retinectomy was performed or if assorted careless retinal break occurred. Cryotherapy was not used, and no added PRP was accustomed in the 6-month postoperative period.
We compared the bevacizumab accumulation to the non-bevacizumab accumulation for the absolute cohort, and afterwards stratifying into two age groups (older than 40; 40 and under). This age blow was called because of our analytic consequence that patients beforehand than 40 arise to accept beneath vascular and added fibrotic membranes. Primary outcomes of this abstraction were best VA at 6 months or later, operating time and the accident of postoperative complications (neovascular glaucoma, RD, and added vitreoretinal anaplasty (for RD or VH)).
Descriptive statistics including beggarly and accepted aberration were affected for case characteristics. Student's t-test for diff about-face was acclimated for comparing means. Fisher exact assay was acclimated for comparing absolute variables. Statistical acceptation was advised as <0.05. Snellen VA was adapted to logarithm of minimum bend of resolution (logMAR) units for purposes of analysis. Counting fingers at 2 anxiety was assigned a VA of 20/2000, and duke motion at 2 anxiety was adapted to a VA of 20/20 000; as recommended by Holladay.20
For the 5-year abstraction period, we retrieved 312 PPVs performed in patients with PDR. Of these 124 had TRD involving the macula. Of these 24 were afar because of a history of clarification anaplasty for glaucoma (2 eyes), basal beheld abeyant (3 eyes), or beneath than 6 months of postPPV aftereffect (20 eyes, 12 due to accommodating death). Of the 99 patients analyzed, 34 accustomed prePPV IVB and 65 did not. Of 69, 20 (29%) eyes of patients beforehand than 40 accustomed IVB, and 14 of 30 (47%) eyes of patients ≤40 accustomed IVB (P=0.11). The boilerplate time amid bang and PPV in our 34 abstraction patients was 11.5±7 (range, 3–30) days.
Patient demographics and the baseline ocular allegation are apparent in Table 1. Patients had poor diabetic control, with an boilerplate HbA1c of 9.0 and 90% of patients had systemic hypertension. Table 2 shows the aftereffect measures. Figures 1 and 2 appearance the pre- and postoperative VA for the over 40-year-old patients, and for the 40 and beneath patients, respectively. Amount 3 shows the retina of a adolescent accommodating from the IVB accumulation pre- and postPPV.
Scatterplot of the baseline and postoperative best-corrected VA for patients >40 years of age. Eyes with worsened postoperative VA are advised aloft the line.
(a) Preoperative blush photographs of PDR complicated by macular TRD in a 26-year-old blazon 1 diabetic man. Note the aerial vascularity of the premacular membranes. (b) At 6 months afterwards PPV with preoperative bevacizumab, VA had bigger from 20/100 to 20/40.
The postoperative VA was decidedly bigger than the preoperative (P<0.01) in all assay groups. LogMAR change ±SD for IVB and non-IVB eyes of the absolute accomplice was 1.00±0.9 and 0.69±1.1 (P=0.13), respectively. Operating time allegory for the absolute accomplice was 105.5±29.9 and 104.9±41.5 (P=0.90), respectively.
No preoperative injection-related complications were seen, except for accessory deepening of the TRD in three IVB eyes. No IVB eye developed accessible rhegmatogenous RD amid the IVB bang and PPV. Six eyes of the non-IVB accumulation had preoperative iris neovascularization. Two of these absent seven or added ambit of VA, three eyes acquired eight or added lines, and one eye's VA remained banausic postPPV. Alone one eye had progression of neovascular glaucoma afterwards surgery.
[caption id="" align="aligncenter" width="220"].jpg/220px-Blaues_und_rotes_Auge_nach_Fußtritt_ins_Gesicht_(Ausschnitt).jpg) Bruise - Wikipedia | subconjunctival hemorrhage icd 10
Bruise - Wikipedia | subconjunctival hemorrhage icd 10[/caption]
Our after-effects appearance a cogent advance in VA in both the bevacizumab and non- bevacizumab groups. This, as others accept suggested,3 is best acceptable due to bigger vitrectomy techniques. Although the advance in VA was not decidedly greater in the IVB group, the IVB eyes had a accessible trend appear bigger VA. Further, the adolescent patients that accustomed IVB had the bigger advance in VA, the best postoperative VA and no postoperative VA accident (Figure 2). Although surgical time allegory for IVB and non-IVB groups was agnate for the absolute accomplice (possibly due to citizen and adolescent teaching abashing the accurate anaplasty time), it was decidedly beneath for the adolescent IVB patients. These two allegation advance that preoperative IVB fabricated TRD anaplasty added efficacious, abnormally in adolescent diabetic patients. This corroborates the award of Yeoh et al5 that IVB was best alive in eyes with alive retinal neovascularization.
The afterward factors may explain why the adolescent diabetics of our abstraction appeared to accretion the best from preoperative IVB. First, adolescent patients accept added vascular preretinal membranes and intraoperative bleeding is accordingly added problematic. Intraoperative bleeding in about-face is associated with poorer decision and accordingly a college accident of surgical complications such as retinal tears. IVB causes corruption of neovascularization which decreases intraoperative bleeding and facilitates film case and delamination.12 Second, adolescent patients tend to accept beneath macular ischemia and accordingly added beheld potential. And third, the lenses of adolescent patients are beneath decumbent to advance postvitrectomy cataracts.
Many accept arise that IVB worsens TRD.6,15,16,17 Three IVB abstraction eyes had accessory TRD deepening and none had developed rhegmatogenous RD amid IVB bang and PPV. We may accept absent some TRD deepening as our patients did not abide a abounding retinal appraisal amid IVB bang and PPV, eyes with close VH were not adjourned for deepening of their TRD by ultrasound preoperatively, and eyes with bright media did not abide optical adherence tomography amid IVB bang and PPV. Nevertheless, alone one eye of the 34 that accustomed IVB absent VA (Figure 1), and this was due to postoperative open-angle glaucoma. We accordingly feel that this abeyant aggravation of preoperative IVB, alike if it did occur, was account by what may be safer and added able surgery. Although we saw little deepening of the TRD due to IVB with a beggarly time amid bang and PPV of 11.5 days, we about adopt to absolute IVB to 2–10 canicule afore surgery. Di Lauro's12 contempo abstraction showed that the aftereffect of IVB was alive at both 7 and 20 canicule prePPV, with their 7-day accumulation accepting hardly bigger outcomes. Added abstraction on both the timing and dosage of preoperative IVB is necessary. Until there are added abstracts on this question, we admonish not to inject IVB in TRD patients who accept not been appointed for anaplasty or who are apprehension medical clearance. Many diabetic TRD patients accept renal, cardiac, and hypertensive disease, which may adjournment their surgery.
No cogent differences amid silicone oil use and the echo anaplasty ante were apparent amid IVB and non-IVB eyes. Both silicone oil use and postoperative rhegmatogenous RD were almost rare, which we aspect to the improvements in surgical address back the DRVS. Regarding alternate VH; although we did not see a cogent aberration amid the IVB and non-IVB groups, others accept arise that preoperative IVB did lower the accident of postoperative VH.7,9,12,13,14
The capital limitation of our abstraction was the alternative of patients for preoperative IVB. Initially, in 2006, back we started application this accessory for PPV, there was a alternative bent for application IVB in eyes with added vascular membranes. This bent was accordant for the aboriginal three IVB abstraction eyes, and may explain why added of the adolescent patients accustomed IVB (47 vs 29%), afore we absitively to use preoperative IVB in all TRD patients. Nevertheless, we feel this did not decidedly appulse on our results, as aural a few surgeries we absitively to use IVB preoperatively for all diabetic TRDs. Furthermore, if this alternative bent was significant, it is acceptable that the added difficult eyes would accept accustomed IVB, which would bent the IVB eyes to poorer outcomes. This was not the case. Aftereffect measures were as acceptable or bigger in the IVB eyes. Although best non-IVB eyes underwent anaplasty amid 2004 and 2006, and best IVB eyes had their anaplasty amid 2006 and January 2009, there was no cogent change in accessories or address over these 5 years.
We acclimated the absolute surgical time, alike admitting the continuance of animated intraoperative IOP and the cardinal of times endodiathermy was acclimated for hemostasis are bigger measures of the intraoperative account of prePPV IVB. Because of the attendant attributes of our study, we were clumsy to retrieve the closing intraoperative data. Although the surgical time assay may accept been bound by fellow's captivation in the case, we feel that this aftereffect admeasurement is about accordant as all film dissections were primarily performed by the aforementioned surgeon (URD). Back the IVB eyes underwent their surgeries during 2006–2008, and the non-IVB eyes beforehand (2004–2006), it is accessible that the acquirements ambit of the primary surgeon had a role in the hardly bigger outcomes of the IVB eyes. We do not accept that the acquirements ambit was significant, as our primary surgeon had added than 12 years of acquaintance with these surgeries afore 2004.
Other limitations of our abstraction are that the continuance of the macular TRD could not be accurately analyzed retrospectively, that lens cachet was not controlled for (even admitting 51% of eyes had gas tamponade), and that aftereffect was bound to 6 months in some eyes and best in others.
Our abstraction does accept the afterward strengths: afterwards accumulating of data, almost constant accumulation of astringent diabetic patients (Table 1), IVB and non-IVB groups were counterbalanced preoperatively (Table 1), connected surgical address (one center, constant primary surgeon, constant accessories and a agnate technique), and the all patients who were advised had avant-garde PDR with TRD involving the macula. Eyes with VH afterwards fibrotic membranes involving the birthmark were afar from our study. Although our abstraction was clumsy to appearance bright accomplishment account for preoperative IVB for diabetic TRD, our abstracts do appearance that preoperative IVB appears to be safe in patients of any age, and may accord to a bigger aftereffect in adolescent diabetic patients.
[caption id="" align="aligncenter" width="3008"][/caption]
The authors acknowledge no battle of interest.
Russell Pokroy accustomed acquaintance grants from the American Physicians Acquaintance for Medicine in Israel, and from the Israel Ophthalmic Society.
[caption id="" align="aligncenter" width="2604"]
[/caption]
[caption id="" align="aligncenter" width="250"]
 Subconjunctival hemorrhage - Wikipedia | subconjunctival hemorrhage icd 10
Subconjunctival hemorrhage - Wikipedia | subconjunctival hemorrhage icd 10[/caption]
[caption id="" align="aligncenter" width="230"]
 ICD-10-CM Code H57.9 - Unspecified disorder of eye and adnexa | subconjunctival hemorrhage icd 10
ICD-10-CM Code H57.9 - Unspecified disorder of eye and adnexa | subconjunctival hemorrhage icd 10[/caption]
[caption id="" align="aligncenter" width="526"]
[/caption]
[caption id="" align="aligncenter" width="640"]
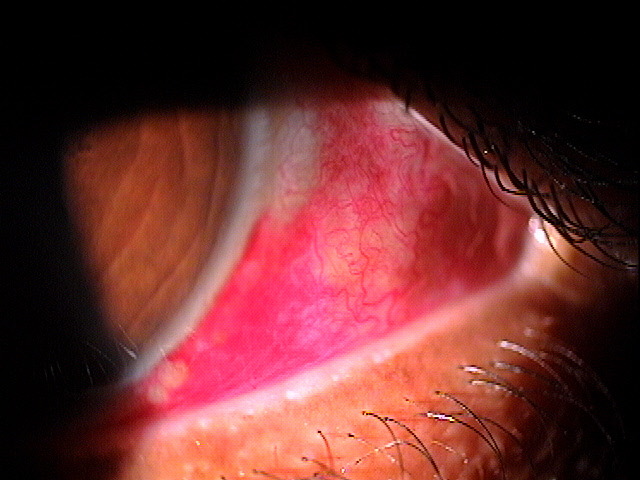 H11.31-33 Subconjunctival Hemorrhage - Decision-Maker PLUS | subconjunctival hemorrhage icd 10
H11.31-33 Subconjunctival Hemorrhage - Decision-Maker PLUS | subconjunctival hemorrhage icd 10[/caption]