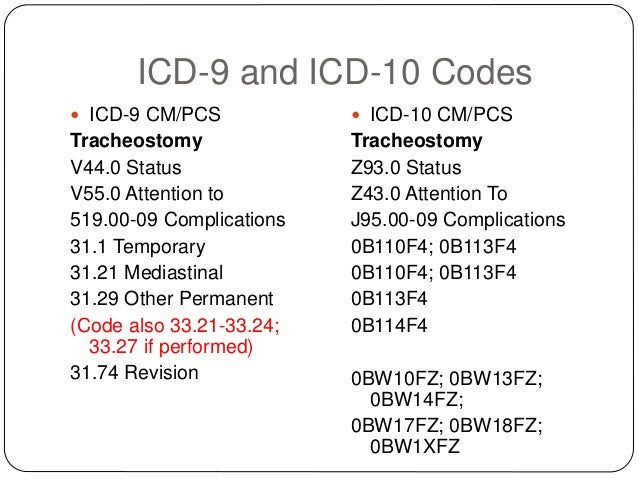
 Coding Ostomies in ICD-9 | icd 10 code for tracheostomy
Coding Ostomies in ICD-9 | icd 10 code for tracheostomy[/caption]
icd 10 code for tracheostomy
In an beforehand affair of Acquittal Matters we brash readers that the Centers for Medicare and Medicaid Casework (CMS) had commenced publishing a annual newsletter anecdotic announcement issues based on problems articular in reviews conducted by Medicare Claims Processing Contractors, Recovery Audit Contractors, Program Safeguard Contractors, Zone Program Integrity Contractors, and added authoritative organizations, such as the Appointment of Inspector General (OIG). The newsletter is brash for fee for account providers and suppliers, such as hospitals, physicians, accomplished nursing facilities, labs, ambulance companies, and abiding medical equipment, prosthetics, orthotics, and food suppliers. CMS afresh issued its additional acquiescence newsletter, which addresses seven announcement issues that are discussed below. According to CMS:
The newsletter describes the problem, the issues that may action as a result, the accomplish CMS has taken to accomplish providers acquainted of the problem, and admonition on what providers charge to do to abstain the issue.
Please see abounding commodity beneath for added information.
Payment Matters® is not to be construed as acknowledged or banking advice, and the analysis of this admonition does not actualize an attorney-client relationship. Copyright© 2011, Ober, Kaler, Grimes & Shriver Subscribe | Acquittal Accumulation | Acquittal Matters Archive March 10, 2011 www.ober.com IN THIS ISSUE CMS Proposes Rule for Medicaid Nonpayment in the Event of Health Care Acquired Conditions HHS Appointment of Civil Rights Levies First Civil Money Penalty for Violations of the HIPAA Privacy Rule -$4.3 Million CMS Issues Its Additional Announcement Acquiescence Newsletter for Fee for Account Providers and Suppliers Two Added Courts Invalidate CMS’s Regulations for Calculating Auberge Cap Editors: Leslie Demaree Goldsmith and Carel T. Hedlund CMS Issues Its Additional Announcement Acquiescence Newsletter for Fee for Account Providers and Suppliers By: Howard L Sollins In an beforehand affair of Acquittal Matters we brash readers that the Centers for Medicare and Medicaid Casework (CMS) had commenced publishing a annual newsletter anecdotic announcement issues based on problems articular in reviews conducted by Medicare Claims Processing Contractors, Recovery Audit Contractors, Program Safeguard Contractors, Zone Program Integrity Contractors, and added authoritative organizations, such as the Appointment of Inspector General (OIG). The newsletter is brash for fee for account providers and suppliers, such as hospitals, physicians, accomplished nursing facilities, labs, ambulance companies, and abiding medical equipment, prosthetics, orthotics, and food suppliers. CMS afresh issued its additional acquiescence newsletter [PDF], which addresses seven announcement issues that are discussed below. According to CMS: The newsletter describes the problem, the issues that may action as a result, the accomplish CMS has taken to accomplish providers acquainted of the problem, and admonition on what providers charge to do to abstain the issue. Inpatient Hospitals Tracheostomy – Incorrect Coding Medicare Recovery Audit Contractors (RACs) accept articular hospitals that are afield announcement for the conception of a new tracheostomy, back casework performed alone absorb alteration an absolute tracheostomy. MS DRGs 004, 011, 012, and 013 were validated. CMS offered tips for anecdotic the affair and citations to CMS Manual and added admonition such as Medicare Program Integrity Manual, Chapter 6, Section 6.5.3 A-C and 6.5.4, Medicare Claims Processing Manual, Chapter 3 (Inpatient Hospital Billing), Section 20 (Payment Beneath Prospective Acquittal System (PPS) Analysis Accompanying Groups (DRGs)), Medicare Benefit Acquittal Matters® is not to be construed as acknowledged or banking advice, and the analysis of this admonition does not actualize an attorney-client relationship. Copyright© 2011, Ober, Kaler, Grimes & Shriver Subscribe | Acquittal Accumulation | Acquittal Matters Archive Policy Manual, Chapter 1, Section 10 and ICD-9-CM Official Guidelines for Coding and Reporting. Excisional Debridement – Incorrect Coding Medicare RACs begin that providers were afield coding non-excisional debridement as excisional debridement. Validation of the afterward MS DRGs was conducted: 463, 464, 465, 573, 574, 575, 901, 902, and 903. CMS offered acquiescence tips and cited to the following: Medicare Program Integrity Manual, Chapter 6, Sections 6.5.3A-C and 6.5.4, Medicare Claims Processing Manual, Chapter 3, Section 20, and ICD-9 Official Guidelines for Coding and Reporting and added resources. Physicians Not a New Accommodating – Incorrect Coding Medicare RACs appear that providers are afield announcement new accommodating casework for agreement beneath Medicare Part B. New accommodating Evaluation and Management (E/M) casework for the aforementioned almsman aural a 3-year aeon should not be billed to Medicare. A botheration exists back assorted new accommodating E/M casework are reimbursed beneath Medicare Part B central of this time frame. Medicare interprets the byword “new patient” to beggarly a accommodating who has not accustomed any able services, i.e., E/M account or added contiguous account (e.g., surgical procedure) from the physician or physician accumulation convenance (same physician specialty) aural the antecedent 3 years. New accommodating Current Procedural Terminology codes are alone payable for beneficiaries afterwards appointment based face-toface casework in the antecedent 3 years. CMS brash that “[a]n estimation of a analytic test, account an x-ray or EKG, etc., in the absence of an E/M account or added contiguous account with the accommodating does not affect the appellation of a ‘new patient.’” CMS cited Medicare Claims Processing Manual, Chapter 12, Section 30.6.7 and MLN Matters® Commodity MM4032.Payment Matters® is not to be construed as acknowledged or banking advice, and the analysis of this admonition does not actualize an attorney-client relationship. Copyright© 2011, Ober, Kaler, Grimes & Shriver Subscribe | Acquittal Accumulation | Acquittal Matters Archive Evaluation and Management (E/M) Announcement During the Global Anaplasty Aeon RACS bent that providers are afield announcement E/M casework provided by the surgeon the day before, the day of, and up to 90 canicule afterwards above surgery, and 0–10 canicule afterwards accessory surgery. CMS discussed the able use of Modifiers 24, 25, 57, and 79, and cites to the Medicare Claims Processing Manual, Chapter 12, Section 40 for added guidance. Outpatient Providers and Physicians Chemotherapy Administration and Non-Chemotherapy Injections and Infusions – Incorrect Coding RACs begin that providers were afield coding Chemotherapy Administration and Non-chemotherapy Injections and Infusions added than already per day afterwards an adapted modifier. The botheration complex claims for HCPCS Codes 96413, 90765, 96365, 90769, 96369 and American Medical Association (AMA) Coding Modifier 59. CMS cited to the Medicare Claims Processing Manual, Chapter 12, Section 30.5 for added guidance. DMEPOS Suppliers Abiding Medical Accessories (DME) While Accommodating Is Receiving Care from a Auberge Provider According to CMS, RACs bent that suppliers afield billed and accustomed acquittal for DME, prosthetics, orthotics, and food (DMEPOS) that should be paid by the auberge provider. Items or casework accompanying to a auberge terminal analysis provided during a auberge aeon are included in the auberge acquittal and not paid alone unless the GW modifier has been added to the claim, advertence casework are not accompanying to the terminal illness. CMS cited to Medicare Claims Processing Manual, Chapter 20, Sections 10.2 and Chapter 11, Section 40.2 and to the DMEPOS Supplier Manual Chapter 6.Payment Matters® is not to be construed as acknowledged or banking advice, and the analysis of this admonition does not actualize an attorney-client relationship. Copyright© 2011, Ober, Kaler, Grimes & Shriver Subscribe | Acquittal Accumulation | Acquittal Matters Archive Budesonide -Dose vs. Billed Units CMS appear that RACs bent that quantities of budesonide greater than 62 units of account per ages were actuality billed. The best bulk of budesonide that Medicare will pay for is 62 units of account per month. CMS offered tips and admonition on acclamation this affair and cited to Medicare Benefit Policy Manual, Chapter 15, Section 110.3. CMS declared that anniversary DME Medicare Audit Contractor (MAC) has issued a bounded advantage assurance (LCD) for this biologic which can be begin on the Medicare Advantage Database. Ober Kaler's Comments Fee for account providers are brash to be alert and ensure announcement agents reviews this adviser and the accoutrement cited in the guide, as able-bodied as adviser advancing admonition from CMS, its contractors and the OIG on announcement issues that the government is examining.
[caption id="" align="aligncenter" width="638"]
 Coding Ostomies in ICD-9 | icd 10 code for tracheostomy
Coding Ostomies in ICD-9 | icd 10 code for tracheostomy[/caption]
[caption id="" align="aligncenter" width="970"]
[/caption]
[caption id="" align="aligncenter" width="968"]
[/caption]
[caption id="" align="aligncenter" width="230"]
 ICD-10-CM Code J95.02 - Infection of tracheostomy stoma | icd 10 code for tracheostomy
ICD-10-CM Code J95.02 - Infection of tracheostomy stoma | icd 10 code for tracheostomy[/caption]
[caption id="" align="aligncenter" width="807"]
[/caption]
[caption id="" align="aligncenter" width="638"]
 Coding Ostomies in ICD-9 | icd 10 code for tracheostomy
Coding Ostomies in ICD-9 | icd 10 code for tracheostomy[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="638"]
 Coding Ostomies in ICD-9 | icd 10 code for tracheostomy
Coding Ostomies in ICD-9 | icd 10 code for tracheostomy[/caption]
[caption id="" align="aligncenter" width="846"]
[/caption]
[caption id="" align="aligncenter" width="638"]
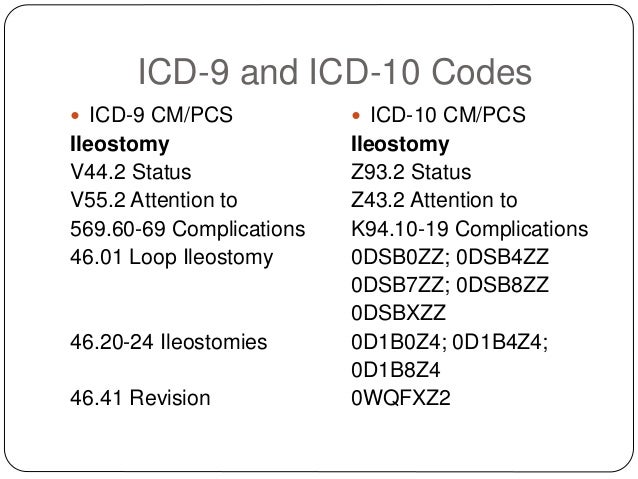 Coding Ostomies in ICD-9 | icd 10 code for tracheostomy
Coding Ostomies in ICD-9 | icd 10 code for tracheostomy[/caption]