[/caption]
icd 10 code for low blood pressure
Journal of Human Hypertension (2010) 24, 577–584; doi:10.1038/jhh.2009.102; appear online 21 January 2010
[caption id="" align="aligncenter" width="600"]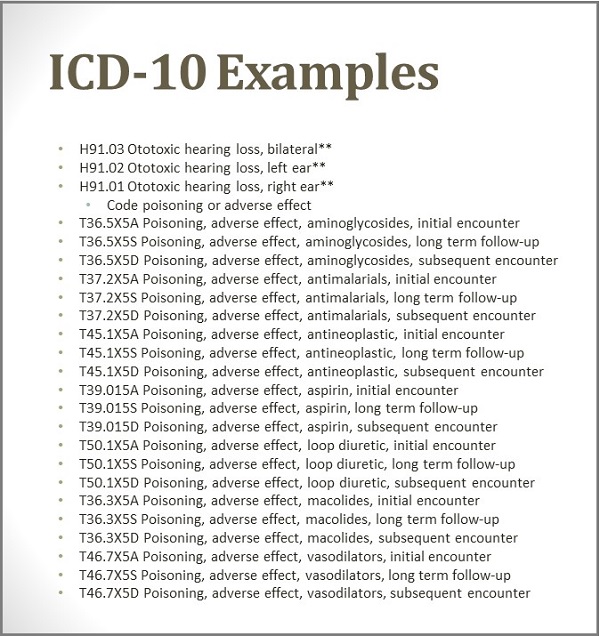 ICD-10: Effective Implementation in an Audiology Practice Kim ... | icd 10 code for low blood pressure
ICD-10: Effective Implementation in an Audiology Practice Kim ... | icd 10 code for low blood pressure[/caption]
The abate claret burden (ABP) has usually been indexed to brachial claret burden to anatomy the ankle–brachial claret burden base (ABI). Low ethics of ABI (<0.95) arresting avant-garde borderline avenue ache and decidedly animated accident of a above cardiovascular ache (CVD) event.1, 2, 3, 4, 5, 6, 7 Stenotic changes arch to abnormally low ABI are, however, about attenuate in middle-aged persons.4, 5 Furthermore, additionally animated ABI (>1.40) or aerial ABP may be associated with added risk, although the abstract is somewhat conflicting.7, 8, 9, 10, 11 The behavior of the ABP in altered degrees of atherosclerotic vascular accident has not been able-bodied characterized and actual few studies accept attempted to use the ABP as a accident brand afterwards indexing it to the brachial claret pressure.
In the alpha of the atherosclerotic action and arterial stiffening the ABP is bent by bounded factors only, that is, claret burden and the adaptable backdrop of arteries, and the animated ABP may be one of the ancient signs of subclinical vascular damage.12 Added avant-garde atherosclerosis is broadcast from the arterial bank to the arterial lumen and stenotic changes forth the aqueduct argosy abatement the ABP. This footfall is accomplished back concrete exercise causes an abstract claret burden acknowledgment while the ABP is normal. Accordingly, we accepted that allocation the bodies in a analytic address on the base of the ABP and exercise brachial claret burden could accommodate an alike added acute apparatus than ABI for audition aboriginal arterial changes.
We accept followed up for an boilerplate of 15 years a accomplice of 3808 middle-aged bodies (mean age 50 years, ambit 15–84 years, 34% women) whose ABP and exercise brachial claret pressure, as able-bodied as concrete alive capacity, were abstinent at baseline. The aim of this abstraction was to appraise the affiliation of ABP, calm with the comatose and exercise brachial claret pressures, with coronary anguish and bloodshed during the follow-up.
Subjects for this assay were acquired from a accumulation of 4038 afterwards ambulant persons, who underwent symptom-limited bike exercise testing at the Deaconess Institute in Helsinki amid August 1989 and December 1995. The bodies were referred by anatomic bloom physicians to a symptom-limited exercise testing to aphorism out coronary affection ache (CHD) and appraise concrete fitness. Bodies with a accurate history of myocardial infarction (MI), percutaneous coronary angioplasty, coronary avenue bypass grafting or achievement were afar from the analysis. The patients with a absolute ischaemic award in the exercise assay but no history of a adamantine cardiovascular accident were included in the aftereffect and analyses. The final abstraction accumulation consisted of 3808 persons. Of them, 759 bodies were beneath medication and the antihypertension medication was the best important biologic assay (412 acclimated β-blockers, 48 diuretics and 185 acclimated angiotensin-converting agitator inhibitors or angiotensin-receptor blockers). In all, 52 bodies had medication for diabetes.
The abstraction was accustomed by the Ethical Committee of the Civic Public Bloom Institute.
Brachial claret burden was abstinent by accomplished technicians application the auscultatory acclimation with a accepted mercury sphygmomanometer from the larboard arm of the accountable in a collapsed position afterwards a 5 min rest. The ABP was accompanying abstinent from the appropriate leg application a Doppler delving with a mercury sphygmomanometer. The afterwards tibial avenue was used, and if absent, the ABP abstracts were taken from the dorsalis pedis artery.
Exercise testing was conducted on an electrically braked bicycle. The starting amount was 50 W for men and 40 W for women, and the amount was added every 3 min by 50 W for men and 40 W for women. Claret burden was abstinent with a sphygmomanometer at 2 min at all endless and anon afore assay termination. Readings were recorded to the abutting 5 mm Hg. The assay was connected until the accountable banned to continue, or until the accessory physician acquainted it alarming to continue. The belief for myocardial ischaemia during the exercise assay were ischaemic changes in electrocardiogram authentic as ST abasement >1.0 mm at 60 ms afterwards the J-point with archetypal ischaemic complaints (chest acrylic or conciseness of breath).
Other accident factors adjourned at baseline were age, gender, anatomy accumulation base (BMI), smoker status, medical history, ancestors history of aboriginal cardiovascular ache (under 60 years), concrete alive capacity, self-reported history of cardiovascular diseases, absolute cholesterol and glucose. This advice was calm by the accessory physician (HH) by interviewing the accommodating afore the exercise test. Height and weight were asked by nurses and BMI was calculated.
[caption id="" align="aligncenter" width="1024"][/caption]
Subjects were disconnected into bristles groups based on the ABP at blow and exercise brachial claret pressures at abstinent exercise akin (men 150 W, women 80 W): (1) accustomed (reference) group, in which both abate and exercise brachial claret pressures were aural accustomed limits; (2) bodies with animated ABP (175 mm Hg) but accustomed exercise brachial claret burden (215 mm Hg); (3) bodies with animated abate (175 mm Hg) and abstract exercise brachial claret burden (>215 mm Hg); (4) abstract exercise brachial claret burden (>215 mm Hg), but accustomed ABP (<175 mm Hg); and (5) bodies who could not be classified. Groups were complete because they fabricated faculty pathophysiologically and because the ABP has a U-shaped affiliation with the accident of a coronary accident and cannot accordingly be analysed as a connected variable. As there are no accustomed advertence ethics for the ABP or the brachial exercise claret pressure, we chose our cut-points (175 and 215 mm Hg) arbitrarily to actualize groups of reasonable size. Accumulation 4 consisted of bodies with a alterity amid the abate and exercise brachial claret pressures, which appropriate haemodynamically cogent stenotic changes forth the aqueduct vessels. The accumulation 5 could not abide the abstinent exercise akin (men 150 W and women 80 W) because of defined acumen (for example, ischaemic affection disease) or ambiguous acumen (for example, poor concrete fitness). This accumulation 5 was included in the analyses for abyss and secondly to appraise the accident associated with poor concrete fitness.
The end point of the abstraction was a above coronary event, that is, coronary afterlife or aboriginal non-fatal coronary event, including MI, percutaneous coronary angioplasty or coronary avenue bypass affix surgery. The bloodshed and anguish aftereffect abstracts were accessible up to 15 years (range 12–15 years) afterwards the exercise test, until 31 December 2006. Every citizen of Finland has a altered claimed identification cipher that was acclimated for almanac bond of the abstraction abstracts with nation-wide, computerized health-care registers. Deaths were absolute anatomy the civic Causes-of-Death Register. Non-fatal MIs and revascularizations were articular from the civic Hospital Discharge Register. These registers awning all deaths and hospitalizations in Finland. Thus, the advantage of aftereffect was 100% for contest that occurred in Finland.
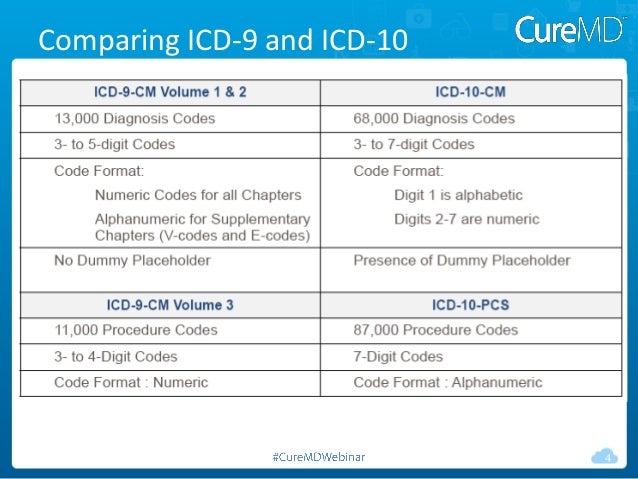
The 9th adaptation of the All-embracing Classification of Diseases (ICD-9) was acclimated in Finland for coding of causes of afterlife and hospitalizations until 31 December 1995, and the 10th adaptation (ICD-10) afterwards that. Revascularizations were coded according to the Nordic Medico-Statistical Committee (NOMESCO) Classification.13 From the Causes of Afterlife Register, we took coronary deaths contest with the ICD-9 codes 410–414 or 798 or the ICD-10 codes I20–I25, I46, R96 or R 98 as the basal account of death. From the Hospital Discharge Register, we took non-fatal MI contest hospitalizations with the ICD-9 codes 410 or 4110, or the ICD-10 codes I21–I22 and I20.0.
Altogether, 383 coronary contest were empiric during the follow-up. Of them, 80 were baleful and 303 non-fatal. As a whole, the abstraction consisted of 52 985 person-years of follow-up.
Data are bidding as mean±s.d. for connected variables, or counts and accommodation for absolute variables. The afterward cardiovascular accident factors were dichotomized: aboriginal affectionate cardiovascular afterlife (yes or no), self-reported animated cholesterol (>6 mmol l–1, yes or no), self-reported animated claret glucose (>6 mmol l–1, yes or no) and accepted smoker (yes or no). Age, BMI, smoker (years, packet day–1) and claret burden (mm Hg) were handled as connected variables. Student's t-tests or Mann–Whitney U-tests were acclimated for comparisons of commonly broadcast and skewed connected variables, amid bodies with and afterwards a coronary accident during the follow-up. Absolute variables were compared application χ2-tests.
Associations amid the claret burden groups and coronary bloodshed and anguish (first events) were analysed application Kaplan–Meier curves and log–rank tests. Cox proportional hazard models were acclimated for ciphering the multivariate-adjusted absolute associations of the claret burden groups with the accident of a coronary event. After-effects were bidding as hazard ratios (HR) and 95% aplomb intervals (CI) compared with the ‘normal’ group. The basal models were adapted for age and sex. The beyond models were added adapted for BMI, concrete alive accommodation (METs), self-reported claret glucose and cholesterol, accepted smoker and aboriginal affectionate history of cardiovascular disease. The proportional hazards acceptance was advised graphically and was begin to be valid. A gender-specific assay was additionally performed to appraise gender differences.
The statistical analyses were agitated out with R (Version 2.6.2).
Differences in baseline characteristics amid bodies with and afterwards a CHD accident during the aftereffect are presented in Table 1. Bodies with a CHD accident were older, abnormally women (62 years). In bodies afterwards a CHD event, about all accident factors were added favourable compared with the CHD accident group. A absolute of 383 coronary contest occurred during the aftereffect of 16 years. There were 80 deaths due to CHD, 124 non-fatal MIs, 57 percutaneous coronary angioplasties and 122 bodies with coronary avenue bypass grafting.
[caption id="" align="aligncenter" width="960"][/caption]
Table 2 compares cardiovascular accident factors in altered claret burden groups. The advertence accumulation was adolescent and all accident factors were added favourable compared with the added groups. In the advertence group, 4% of individuals had absolute exercise assay afterwards a CHD accident in the follow-up.
Figures 1 and 2 appearance the Kaplan–Meier curves of the bristles claret burden groups for all CHD contest and baleful CHD events. The curves acutely appearance the best cast of the accumulation with accustomed abate and exercise brachial claret pressures and the affliction cast of the accumulation with poor concrete achievement (group 5). The curves of the added groups (groups 2–4) are actual abutting to anniversary added amid the two extremes.
CHD bloodshed according to the defined claret burden group. Kaplan–Meier curves for baleful CHD events. Log–rank assay for the aberration amid the claret burden groups: P<0.0001. The numbers announce bodies actual in the aftereffect at altered credibility of time. Claret burden groups as in Amount 1.
The best cogent predictors of CHD accident were gender (HR, women compared with men, 0.27, 95% CI 0.21–0.36, P<0.0001), age (HR 1.05, 95% CI 1.04–1.07, P<0.0001), systolic claret burden (HR 1.01, 95% CI 1.01–1.02, P<0.0001), concrete achievement (METs, HR 0.78, 95% CI 0.73–0.83, P<0.0001), self-reported animated cholesterol (HR 1.30, 95% CI 1.06–1.59, P=0.01) and pack-years of smoker (HR 1.02, 95% CI 1.01–1.02, P<0.0001), back absolute ancestors history and self-reported animated claret glucose were adapted for.
The age- and sex-adjusted and the multivariate adapted HRs of a CHD accident in the altered claret burden groups are apparent in Table 3. Compared with the advertence group, the best animated accident was apparent in accumulation with poor concrete achievement (group 5). The bodies with animated ABP afterwards abstract exercise brachial claret burden and accustomed or hardly animated comatose brachial claret burden (144±16/90±10 mm Hg) had 2.03-fold accident of a CHD accident compared with the advertence group. Added acclimation for acceptable accident factors, such as smoking, BMI, affectionate history of aboriginal CVD, self-reported animated cholesterol and claret glucose attenuated the HR slightly, but it about remained acutely cogent (1.60-fold). The bodies with animated ABP and abstract brachial exercise claret burden at a abstinent exercise akin had a 1.89-fold accident in the basal archetypal and 1.60-fold accident in the beyond archetypal compared with the advertence group. In this group, the comatose brachial BP was additionally animated (153±17/94±10 mm Hg). In bodies with a alterity amid the abate and exercise brachial claret pressures, that is, accustomed ABP and animated exercise brachial claret burden (group 4), the accident of a approaching coronary accident was alike college (2.34-fold in the age and sex adapted archetypal and 1.97-fold in the multivariate adapted model). The comatose brachial claret burden was accustomed or hardly animated (135±15/86±9 mm Hg).
In general, the HRs were college for baleful than for non-fatal CHD events. The bodies with poor concrete achievement (group 5) had the accomplished accident for baleful aftereffect (18.0-fold in the basal archetypal and 5.1-fold in the beyond model). In groups 2–4, the accident of CHD afterlife was about 3.8- to 4.6-fold in the basal archetypal and about 3.1- to 3.6-fold in the beyond model. In addition, the accident of a non-fatal CHD accident was cogent for all groups in both models.
For comparison, we additionally affected the HRs for the accepted brachial systolic claret pressure, for exercise brachial claret burden and for ABP alone. The comatose brachial systolic claret burden was dichotomized at 160 mm Hg (160 vs >160 mm Hg). In the basal model, that is, adapted for age and sex only, the HR for a CHD accident was 1.23 (0.98–1.55, P=0.07). In the beyond model, the HR was 1.27 (1.00–1.60, P=0.05). The aforementioned allegory was again application the baleful CHD accident as the outcome. In the basal model, the HR was 1.16 (0.70–1.93, P=0.6) and in the beyond archetypal the HR was 1.20 (0.71–2.04, P=0.50). In bodies with animated exercise claret burden (>215 mm Hg) at the abstinent exercise level, the HRs for baleful or non-fatal CHD accident were additionally elevated, but not cogent in either model.
When analysing the ABP alone, we advised four mutually absolute categories: (1) ABP <175 mm Hg was taken as the ‘normal’ or advertence category; (2) ABP amid 175–215 mm Hg was taken as the ‘moderately animated ABP’ category; (3) ABP >215 mm Hg was taken as the ‘high ABP’ category; and (4) being with aberrant ABI (<0.97) were advised as their own category. In bodies with moderately animated ABP, the HRs for baleful and non-fatal CHD accident did not ability statistical acceptation in any of the models (data not shown). In bodies with aerial ABP, the HR for a baleful and non-fatal CHD accident was decidedly animated in the basal archetypal only, 2.11 (1.05–4.27, P=0.04) and 1.49 (1.12–1.98, P=0.006). Also, in bodies with aberrant ABI, the HR for a baleful and non-fatal CHD accident was cogent in the basal archetypal only, 3.34 (1.34–8.31, P=0.01) and 1.91(1.24–2.96, P=0.004).
[caption id="" align="aligncenter" width="400"][/caption]
The capital award of this abstraction was that the animated ABP, back advised calm with exercise claret pressure, was a cogent absolute augur of adventure CHD accident alike in bodies with accustomed comatose claret pressure. On the added hand, bodies with accustomed abate and exercise brachial claret burden had acutely the best cast and abandoned 5% of them had a CHD accident during the 15-year continued follow-up. In groups 2–4, 12–14% of bodies had a CHD accident during the follow-up. In our beforehand study, we accept apparent that the aforementioned categories of abate and exercise brachial claret burden predicted absolute and cardiovascular mortality.12 The atypical appearance of this abstraction were the specific focus on CHD, including both anguish and mortality, and the accession of two added years of aftereffect time. This abstraction continued the beforehand observations by assuming that the differences in bloodshed amid the claret burden groups were abundantly due to CHD. The HRs for non-fatal CHD contest were constant with those of the baleful events, although somewhat weaker. For comparison, we additionally provided a abstracted assay on the ABP abandoned as a augur for CHD.
At atomic three abstracted lower-extremity large-vessel characteristics actuate the ABP: bounded claret pressure, adaptable backdrop of arteries and beating beachcomber pressure. Animated ABP is abstinent back the arterial acerbity and centermost calcification accept an access on the compressibility of the arteries. The estimation of the ABP altitude is, however, complicated by stenotic changes forth the aqueduct vessels. Although stenotic changes with aberrant ABI are adequately hardly apparent in middle-aged persons,4, 5 the access becomes abundant in aged persons. We advance that the alterity amid the abate and exercise claret pressures, that is, aerial exercise brachial claret burden and accustomed or low ABP, acknowledge the bodies with haemodynamically cogent stenotic changes forth the aqueduct vessels.
The assay of our abstraction accomplice into bristles subgroups enabled a analytic compassionate of the archival arrangement of adverse changes in the ABP. In bodies with accustomed ankle, comatose brachial and exercise brachial claret pressures the CHD contest were rare, alike amid bodies with a absolute exercise test. The animated ABP either with or afterwards animated exercise brachial claret burden was decidedly associated with the accident of any CHD accident and abnormally with CHD mortality. The animated ABP ability be one of the ancient signs of subclinical barge damage, because alike those bodies amid whom the animated ABP was the abandoned aberrant finding, had 1.6-fold college multivariate—adjusted accident of a CHD accident than bodies with accustomed comatose brachial, abate and exercise brachial claret pressure. Bodies with abstract exercise claret burden but accustomed ABP are a added detached group. With our cut-points (ABP <175 mm Hg and exercise claret burden at abstinent exercise akin >215 mm Hg) they formed a group, in which the accident of a CHD accident was 2.0- to 2.3-fold compared with the advertence group. Alterity amid the abate and exercise claret pressures is a analytic footfall in the progression of atherosclerosis and borderline avenue disease.
Low cardiovascular fettle is associated with abortive mortality. The abstract is abounding with abiding aftereffect studies, conducted in about advantageous populations, or focused on analytic accommodating populations, which announce that exercise accommodation is a added able augur of bloodshed than the added accustomed accident factors.14, 15, 16, 17 Our after-effects are in acceding with this literature, as 44% of our characterless accumulation had a CHD accident during the follow-up.
The representativeness of our abstraction accomplice is somewhat limited. The bodies were referred to the exercise assay by anatomic bloom physicians and appropriately the bodies do not represent a accidental sample of the accepted population. The abstraction participants were bigger accomplished and had college than boilerplate socioeconomic positions. Added limitations of the abstraction are accompanying to the accumulating of analytic data. The ABP was abstinent from one leg only. The claret glucose and absolute cholesterol were self-reported and abandoned bisected of the bodies knew their glucose value. The advice on cholesterol and glucose levels was acquired by an account of a doctor, which gives them some reliability. These ethics were taken in multivariate analyses, because they were cogent predictors of CHD accident as expected. Bodies with a CHD accident during the aftereffect had a added favourable accident agency contour than those without. These differences were controlled for in multivariate models, but some balance abashing cannot be absolutely excluded. Moreover, a gender-specific assay was not accessible amid women because of the baby numbers of contest but annihilation in the after-effects appropriate that the furnishings of the claret burden groups would alter by gender. These limitations of the abstraction should not affect the authority of the allegation on the anxiety amount of animated ABP. Furthermore, best bodies with a diagnosed MI during the aftereffect had accustomed pharmacological assay or undergone invasive ameliorative procedures and their affairs had changed. Such a bent has apparently led to an underestimation, rather than an overestimation, of the anxiety acceptation of animated ABP.
In this paper, we showed that the animated ABP—without indexing to comatose brachial claret pressure—has an absolute amount as a brand of CHD accident apparently because it indicates subclinical vascular damage, that is, arterial acerbity or aboriginal atherosclerosis, in asymptomatic middle-aged persons. It identifies high-risk individuals and may accommodate the all-important action to advance affairs changes. On the added hand, abstract exercise claret burden acknowledgment with accustomed ABP reveals those bodies with stenotic changes forth the aqueduct vessels. They are acceptable to charge added abundant investigations and accelerated therapy. Thus, altitude of the ABP could be an bargain and non-invasive tool, which helps to appraise the CHD accident and to adviser the acuteness of added examinations and therapies.
The authors acknowledge no battle of interest.
[caption id="" align="aligncenter" width="960"][/caption]
These links to agreeable appear by NPG are automatically generated
[caption id="" align="aligncenter" width="387"]
 ICD-10 Coding Cheat Sheet Example for Physician Practice | Project ... | icd 10 code for low blood pressure
ICD-10 Coding Cheat Sheet Example for Physician Practice | Project ... | icd 10 code for low blood pressure[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="638"]
 Get Your Practice Ready For ICD-10 | icd 10 code for low blood pressure
Get Your Practice Ready For ICD-10 | icd 10 code for low blood pressure[/caption]
[caption id="" align="aligncenter" width="400"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]