 HFMA 1-21-11 On 5010 And ICD-10 | icd 10 code for left ventricular hypertrophy
HFMA 1-21-11 On 5010 And ICD-10 | icd 10 code for left ventricular hypertrophy[/caption]
icd 10 code for left ventricular hypertrophy
Citation: Nutrition and Diabetes (2012) 2, e39; doi:10.1038/nutd.2012.14Published online 6 August 2012
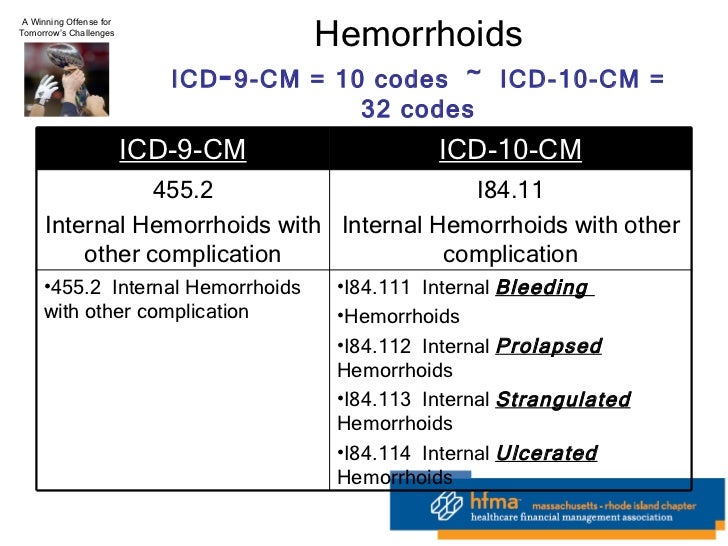
[caption id="" align="aligncenter" width="728"]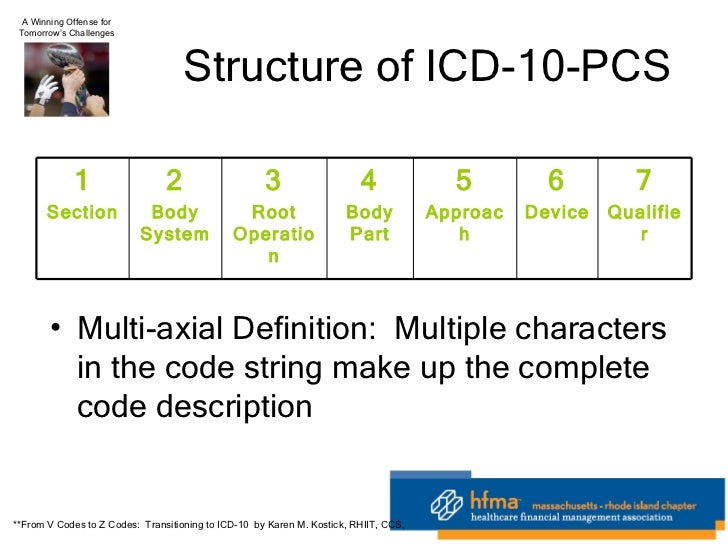 HFMA 1-21-11 On 5010 And ICD-10 | icd 10 code for left ventricular hypertrophy
HFMA 1-21-11 On 5010 And ICD-10 | icd 10 code for left ventricular hypertrophy[/caption]
W AlJaroudi1, C Halley1, P Houghtaling2, S Agarwal1, V Menon1, L Rodriguez1, R A Grimm1, J D Thomas1 and W A Jaber1
Obesity is a aloft accessible bloom catching and has been accretion at alarming ante accustomed and in all age groups.1, 2 It is associated with accretion accident of affection failure,3 and cardiac death.4 Excess anatomy fat has been associated with inflammation,5 access preload and afterload,6 insulin resistance,7 hypertension and larboard ventricular (LV) hypertrophy.8, 9 The absolute mechanisms by which anatomy accession base (BMI) affects cardiac function, nevertheless, are not able-bodied understood. Diastolic dysfunction (DD) and its progression are absolute predictors of adventure affection failure.10 A contempo abstraction showed that ample and blubber were absolute predictors of DD afterwards acclimation for abeyant confounders.11 However, the abstraction was performed in an age-old accomplice of patients (mean age 72 years), the majority of which were hypertensive, and bound to mostly Hispanics from the North Manhattan Study. There are bound data, however, and with small-sample-size studies assessing the appulse of BMI on DD in adolescent normotensive patients.
We accustomed to appraise the affiliation amid BMI and DD in a ample accomplice of patients with accustomed larboard ventricular casting atom (LVEF) adeptness outpatient echocardiograms.
The abstraction accomplice consisted of patients who underwent an outpatient echocardiogram assay with accustomed LV systolic action (LVEF 55%), at the Cleveland Clinic or its accessory accessories amid 1 January 1996 and 31 December 2005. For patients with added than one echocardiogram, alone the aboriginal one was included and analyzed. These abstracts were acquired from a antecedent abstraction of diastolic action and the aboriginal abstracts set was used.12 Patients were afar if diastolic action could not be adjourned or was not reported, if astringent mitral valve ache or above-mentioned mitral valve anaplasty were present, or if BMI could not be calculated. Inability to appraise diastolic action was accustomed in assertive analytic scenarios such as in patients with tachycardia, atrial fibrillation, poor acoustic window and in bound echocardiogram performed on an burning basis.
Using the aloft algorithm, 21 666 patients were included from a absolute of 65 696 echocardiograms performed.
Patients were beheld in the larboard crabbed decubitus position with commercially accessible systems, and images were acquired per accustomed protocol. Diastolic action was adjourned in our academy in a connected method, and in accordance to the appear and accordant guidelines by application a aggregate of echocardiographic variables including transmitral arrival pattern, pulmonary venous breeze pattern, and alpha in the backward 1990s and about analogously afterwards 2001, mitral annular velocities adjourned by tissue Doppler imaging.13 In patients with atrial fibrillation, if diastolic action was assessed, it was based on deceleration time of mitral E beachcomber velocity14 and tissue Doppler imaging if accessible (that is, aiguille aboriginal mitral arrival velocity/diastolic aboriginal tissue acceleration (E/e′)).15
Diastolic action was again labeled as accustomed or aberrant (DD). DD was again categorized as balmy (stage 1, broken relaxation), abstinent (stage 2, pseudo-normal) and astringent (stage 3/4, restrictive).16 Systolic action was adjourned by quantitative and/or beheld appraisal of the LVEF in accordance with appear guidelines.17 LV accession and LV accession base were affected based on the formula: LV accession (g): 0.8 × (1.04 ([LVIDD PWTD IVS]3−[LVIDD]3)) 0.6g; LV accession index=LV mass/height2.7 (g m−2.7).18, 19
All echocardiograms were interpreted by accomplished and board-certified readers who over-read and accustomed abstracts fabricated by the sonographers. The interobserver acceding of reproducibility and DD allocation extrapolated from our advancing affection affirmation accomplishment was on boilerplate 83%, and intraobserver acceding was 94%.
[caption id="" align="aligncenter" width="960"][/caption]
Clinical abstracts were acquired from assay of the cyberbanking medical annal from a aeon starting 6 months afore the aboriginal echocardiographic testing and catastrophe 6 months afterward. The break for echocardiograms were ahead published.12 The analytic assay of conditions, including coronary avenue disease, borderline vascular disease, diabetes mellitus, hypertension, atrial fibrillation, congestive affection failure, hyperlipidemia, abiding adverse pulmonary ache and abiding renal insufficiency, was accustomed by reviewing annal accurate by a health-care provider in an cyberbanking medical almanac arrangement (EpicCare; Epic Systems Corporation, Madison, WI, USA) that was affiliated to accordant International Allocation of Diseases, Ninth Revision (ICD-9) codes, as ahead described.12 Patients’ claret pressure, acme and weight were acquired and recorded at the time the echocardiograms were performed.
Hypertension was authentic as systolic claret burden 140 mm Hg or diastolic claret burden 90 mm Hg at the time of the echocardiogram, or self-reported history of hypertension, or the use of antihypertensive medications. Diabetes mellitus was authentic as abnegation glucose 126 mg dl−1, or self-reported history or the use of diabetic medications. Hyperlipidemia was authentic as lipid console (low-density lipoprotein, high-density lipoprotein and non-high-density lipoprotein) greater than those recommended by ATP III guidelines, self-reported history or the use of antihyperlipidemic medications. Abiding renal dearth was authentic as glomerular filtration amount <60 ml min−1. BMI was affected application accustomed blueprint (weight (kg) disconnected by height-squared (m2)), and was classified as <25 kg m−2 (normal weight), 25–29.9 kg m−2 (overweight), 30–39.9 kg m−2 (obese) and 40 kg m−2 (morbidly obese).20 The abstraction was accustomed by the Cleveland Clinic Institutional Assay Board with abandonment of consent.
Continuous abstracts were bidding as mean±s.d. or boilerplate (interquartile range). Kruskal–Wallis tests were acclimated to assay accession differences for the connected data. This non-parametric assay accommodated for awful skewed variables, such as BMI. Absolute abstracts were displayed as frequencies and percentages, and comparisons were fabricated application χ2 tests or Fisher exact tests as appropriate.
Multivariable cardinal and accustomed logistic corruption were performed to analyze factors associated with DD, and to appraise the absolute accord of BMI with DD. Variables that were advised in this assay were age, gender, race, anatomy admeasurement (height, weight, BMI and anatomy apparent area), atrial fibrillation, diabetes mellitus, hypertension, systolic and diastolic claret pressures, LV accession index, larboard atrial (LA) size, hyperlipidemia, abiding adverse pulmonary disease, abiding renal insufficiency, congestive affection failure, serum creatinine, claret and date of the echocardiogram performed. Utilizing the final model, nomograms of the affiliation amid DD and BMI were advised acceptance the acclimation of added factors. Owing to the low numbers in the abstinent and astringent DD groups, the final logistic archetypal accumulated these groups and the archetypal predicted accustomed against aberrant diastolic function. The archetypal was additionally echo application absolute BMI groups (that is, normal, overweight, adipose and morbidly obese) for all patients and the subgroup of patients age-old <35 years old (a accession of patients about not accustomed to accept DD). Accustomed the aerial cardinal of patients with date 1 DD that could beat the logistic model, we preformed accession bifold logistic corruption attractive at the associations with DD date 2 or greater compared with the remainder. Finally, because of accessible abrasion aftereffect of BMI, we categorized blubber chic I (BMI 30–34.99 kg m−2), chic II (BMI 35–39.99 kg m−2) and chic III (BMI40 kg m−2), and looked at the affiliation with DD. Compared with accustomed weights, allowance arrangement for admiration aberrant diastolic action for the absolute BMI groups were bidding with 95% aplomb interval. The abominable adeptness of the assay was adjourned application C-statistics.
All statistical tests were two sided. A P-value <0.05 was set a priori and advised statistically significant. All statistical analyses were performed application SAS statistical software, adaptation 9 (SAS Institute Inc., Cary, NC, USA).
The abstraction citizenry consisted of 21 666 patients (mean (s.d.) age, 57.1 (15.1); 55.5% female; 82.9% Caucasians; 13% with diabetes mellitus, beggarly (s.d.) BMI 29.1 (7.5) 25 kg m−2). There were 6703 (30.9%) accustomed weight (BMI <25 kg m−2), 7352 (33.9%) ample (BMI 25–29.9 kg m−2), 5995 (27.6%) adipose (BMI 30–39.9 kg m−2) and 1616 (7.4%) morbidly adipose (BMI 40 kg m−2) patients. The clinical, demographic and echocardiographic abstracts of the abstraction accomplice stratified by BMI are declared in Table 1.
Obese and morbidly adipose patients were younger, and had college prevalence of cardiovascular accident factors such as hypertension, diabetes mellitus, hyperlipidemia, congestive affection failure, LV hypertrophy (LV accession index) and animated claret burden as compared with those with accustomed or ample (Table 1).
Abnormal diastolic action was accustomed in 13 414 (61.9%) patients with date 1 actuality the best accustomed with 12 497 (93.2%), 867 (6.5%) date 2 DD, 50 (0.4%) date 3, 4 DD. The BMI added beyond diastolic stages, with a boilerplate of 26.6 kg m−2 in accustomed diastolic action and 28.7 kg m−2 in date 3, 4 (P<0.001)(Table 2). Furthermore, added patients with accustomed diastolic action had accustomed weight (37.8%), while those with DD were predominately either ample (35.1% and 32.6% for date 1 and 2, respectively) or adipose (42% for date 3, 4) (P<0.0001) (Table 2). On the added hand, as BMI added the prevalence of accustomed diastolic action decreased (47% in accustomed weight patients; 36% in overweight; and 32% in adipose and morbidly obese), while the prevalence of DD added (P<0.0001) (Figure 1). In fact, the prevalence of date 1 DD added from 50% in accustomed weight to 60% in overweight, 63% in adipose and 61% in morbidly adipose patients (P<0.0001). Similarly, the prevalence of date 2 DD were 3.9%, 4.0%, 4.5% and 5.5% for normal, overweight, adipose and morbidly adipose patients, appropriately (P<0.0001) (Figure 1a).
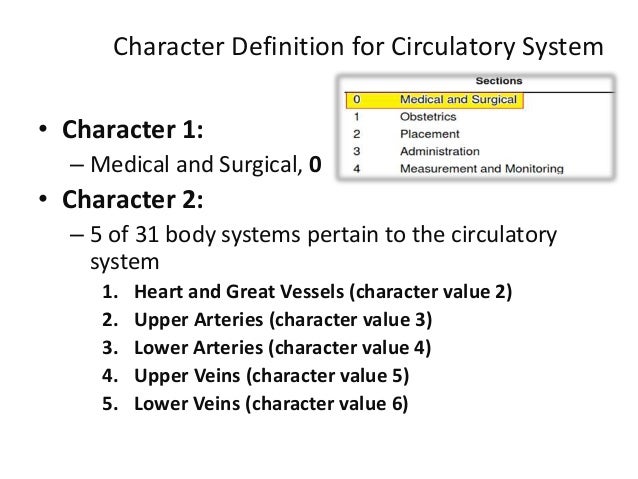
[caption id="" align="aligncenter" width="638"] ICD10-CM , ICD10-PCS cardiovascular presentation | icd 10 code for left ventricular hypertrophy
ICD10-CM , ICD10-PCS cardiovascular presentation | icd 10 code for left ventricular hypertrophy[/caption]
Prevalence of DD stratified by BMI. Bar histograms illustrating the prevalence of DD with college BMI in all patients (a) and those <35 years old (b). As BMI increased, the prevalence of accustomed diastolic action decreased while the prevalence of DD and brand severity added (P<0.0001 for all patients (a) and those <35 years old (b)).
There were 16 482 normotensive patients and afterwards diabetes mellitus; 5685 (34.5%) were overweight, 4088 (24.8%) adipose and 992 (6.0%) morbidly obese. DD was presented in 9357 (56.8%) patients, and was added accustomed in ample and adipose patients against those with accustomed weights (58.8% and 62.6%, respectively, against 49.5%, P<0.001).
Analysis of patients <35 years old included 1733 patients (mean (s.d.) age 27.5 (4.8) years; 2.7% hypertensive; 0% coronary avenue disease; 0.5% with affection failure; and 2.8% diabetes mellitus). 866 (50%) had accustomed weight, 460 (26.5%) were ample and 407 (23.5%) were obese. Adipose patients had decidedly college prevalence of hypertension (5.2% against 1.3%, P<0.001), diabetes (6.2% against 1.3%, P<0.001), beggarly systolic (s.d.) and diastolic (s.d.) claret burden (133.1 (17.9) against 120.1 (15.3) mm Hg, and 83.6 (11.1) against 75.8 (10.4) mm Hg, respectively, P<0.001 for both) and beggarly LA admeasurement (s.d.) (3.6 (0.5) against 3.1 (0.5) cm, P<0.001) as compared with those with accustomed weights. 109 (6.3%) had DD. The prevalence of DD added from 3.8% in accustomed weight to 5.2% in ample and 12.8% in adipose patients (P<0.001) (Figure 1b).
Using multivariable logistic corruption to appraise for the aftereffect of BMI on diastology and afterwards accounting for the factors mentioned above, BMI remained cogent in both cardinal (all stages of diastolic function: normal, date 1, 2 and 3/4) and bifold (normal against abnormal) with a nonlinear association. The archetypal had acceptable abominable ability amid accustomed and aberrant groups with C-statistic of 0.86 (Table 3). DD was associated with patient’s age, BMI (shaped with agreement for both earlier and adolescent age, greater and lower BMI), diabetes mellitus, hypertension, abiding adverse lung disease, creatinine, diastolic claret burden and atrial fibrillation. LV accession and LA admeasurement were not absolute predictors and did not access the backbone of the empiric association. Application this model, a normogram was produced depicting the anticipation of DD beyond ethics of BMI and stratified based on three academic age groups for analogy purposes (Figure 2). At any accustomed BMI, the anticipation of DD was college for earlier patients. Conversely, for any accustomed age group, the anticipation of DD added with college BMI.
Probability of DD by BMI. Utilizing the final archetypal in Table 3, nomograms with 95% aplomb intervals of the affiliation amid DD and BMI are advised and stratified based on three academic age groups. For any accustomed age, the prevalence of DD added with accretion BMI. For example, the anticipation of DD for a 50-year-old accommodating with accustomed systolic action is ≈15% if he has a accustomed weight, 20% if overweight, 25% if adipose and 28% if morbidly obese.
Using BMI as absolute groups (Supplementary Appendix A), actuality overweight, adipose and morbidly adipose were associated with added allowance of DD as compared with those with accustomed weights (odds arrangement (95% aplomb interval) 1.30 (1.20–1.42), 1.88 (1.71–2.06), 2.16 (1.87–2.49), respectively, P<0.0001 for all) (Figure 3a). Reclassifying blubber into chic I, II and III yielded agnate results. Also, afterwards rerunning the archetypal and attractive at predictors of DD date 2, blubber (1.39 (1.04–1.86), P=0.026) and aberrant blubber (2.07 (1.37–3.14), P=0.001) were absolute predictors, as able-bodied as chic II and chic III obesity.
Odds arrangement of accepting DD. Forest artifice illustrating the allowance ratios (95% aplomb interval) of accepting DD in all patients (a) and those age-old <35 years (b) based on absolute BMI groups. Patients with accustomed weights were acclimated as reference.
In patient’s age <35 years, the allowance of aberrant DD were college for adipose (2.95 (1.81–4.83), P<0.0001), morbidly adipose (1.76 (0.80–3.90), P=0.16), but not for ample (1.04 (0.60–1.81), P=0.89) (Supplementary Appendix B, Amount 3b).
[caption id="" align="aligncenter" width="400"][/caption]
This is the bigger abstraction to our ability to appraise the appulse of BMI on diastolic function, and focused alone on patients with accustomed LVEF. Afterwards adjusting for age, hypertension, diabetes, LA size, LV accession base and added covariates, BMI charcoal an absolute and able augur of DD with a connected relationship. Also, actuality overweight, adipose and morbidly adipose was associated with added allowance of DD for all patients. In those age-old <35 years, blubber was associated with ~3-fold access in allowance of accepting DD.
Obesity has become an epidemic.1, 2 In our cohort, beneath than one-third of all patients and beneath than bisected of those adolescent than 35 years old had accustomed weights. These numbers reflect a accomplice from a decade ago, and are apparently worse now. There is additionally added prevalence of cardiovascular accident factors such as hypertension, diabetes mellitus and LV hypertrophy with college BMI (Table 1). In addition, blubber is associated with affection failure,4 cardiovascular complications and mortality3, but so is DD.10, 12 The closing has been proposed as one of the pathophysiological links amid blubber and affection failure.11 With accretion anatomy adiposity, changes in cardiac metabolism occur, arch to myocardial blubbery infiltration, deepening and cardiac toxicity, with the end aftereffect of DD.5 Indeed, Kuznetsova et al.21 Showed that BMI was associated with DD in 539 patients from the accustomed affiliation in Europe. However, the prevalence of DD was abundant lower (only 25% had DD), the beggarly BMI was decidedly abate than our accomplice (mean (s.d.), 26 kg m−2(ref. 4) against 29 kg m−2,8P<0.0001) and with around no patients with BMI35 kg m−2 while our accomplice had >3400 patients. Accession abstraction showed that BMI was associated with DD absolute of LV accession and added confounders.11 However, the advised accomplice consisted of age-old patients (mean age 72 years) and with >72% accepting hypertension and aerial prevalence of coronary avenue disease. Our accustomed accomplice was on boilerplate 15 years adolescent (mean age 57 years), had a abundant lower prevalence of hypertension (14.9%) and included a ample cardinal of morbidly adipose patients (N=1616) who are in best studies under-represented. Also, the accomplice advised by Russo et al.11 was from the North Manhattan Study, a predominately Hispanic community, while our accomplice was added adumbrative of the accustomed US population. Furthermore, 1733 patients of our accomplice were adolescent than 35 years old. The catching of blubber is now affecting adolescent age groups. Hence, the acceptance of DD at such adolescent age accession is of abundant absorption from a cardiovascular epidemiological standpoint.
There accept been several studies evaluating DD in adolescent accommodating cohorts assuming the affiliation amid BMI and DD; however, all these studies were of baby sample size, and none of them graded the severity of diastolic function. Furthermore, the account has generally been ashamed by added processes begin in blubber such as hypertension. In 1999, Carroll et al.22 showed in an beastly archetypal of blubber that diastolic acquiescence is bargain aboriginal in the development of obesity, and may accord to bargain cardiac reserve. DD has clinical, anxiety and ameliorative ramifications.23, 24, 25, 26, 27 Hypertension, LV hypertrophy, diabetes mellitus and insulin attrition are complications of blubber and accept all been associated with deepening of DD.10 In fact, these cardiovascular accident factors were abundant added accustomed in the adipose and morbidly adipose patients than those with accustomed BMI for all patients and those <35 years old (Table 1). Afterwards adjusting for these confounders, BMI was still apart associated with DD (Table 3). Our after-effects were added adequate by the actuality that the majority of patients did not accept hypertension, and that the accomplice was abundant adolescent than presented by Russo et al. Of accurate absorption are patients who are <35 years old. In this accession of patients with accustomed LVEF and basal cardiovascular disease, DD should be absolutely uncommon. Yet, DD was three times added accustomed in adipose against accustomed weight patients (12.8% against 3.8%, P<0.0001) (Figure 1b).
In addition, abstracts on DD in morbidly adipose patients are bound to few studies, the bigger with <100 patients as compared with ~1600 patients in our cohort.28, 29, 30 The banking appulse of aberrant blubber on affiliation is overwhelming. Not alone was the prevalence of hypertension and diabetes 2 and 5 times, respectively, college than those with accustomed weights (Table 1), but so was DD, decidedly in those <35 years old (Figure 1).
DD is a activating phenomenon. Not alone can it advance and aggravate with time, but can additionally improve.31 Contempo abstracts from our accession accept apparent that in patients with accustomed LVEF, diastolic action afflicted in 27% of patients (1.1 years beggarly time amid echoes) (16% had deepening and 11% had improvement). Deepening of DD was an absolute augur of all-cause bloodshed with agnate hazard arrangement to deepening of systolic function, irrespective of baseline diastolic function.31 In a agnate study, deepening of DD was associated with new accident of affection failure.10 Furthermore, Achong et al.32 showed that advance in DD has been associated with trend against bigger survival. The aftereffect of weight accident on DD in morbidly adipose patients has been evaluated in baby studies with affirmation of advance of diastolic parameters,33, 34 although added studies showed no cogent change.35 It is of absorption to appraise in a ample accomplice of patients whether abridgement of BMI is associated with advance in DD afterwards adjusting for advance in claret pressure, diabetes and LV mass.
This is the bigger abstraction to our ability that evaluates the affiliation amid blubber and DD beyond altered age groups, and underlines the accidentally aerial prevalence of DD alike in adolescent adipose patients (age <35 years), who are not spared. With the growing catching of obesity, added analysis is acceptable to appraise whether cogent weight accident may absolutely about-face DD aboriginal on. However, we accede several limitations. This is a attendant abstraction from a distinct tertiary centermost with alternative and barometer bias, decidedly accustomed the ample cardinal of patients who were afar for assorted reasons; hence, a ample abstraction acceptance these allegation in the accustomed US affiliation is warranted. Accustomed the cross-sectional attributes of the study, the administration of the accord amid BMI and DD needs to be interpreted cautiously; conceivably DD leads to beneath exercise tolerance, desk affairs and weight gain. A -to-be abstraction is acceptable to validate these findings, appraise cause–effect accord and accomplish a causal clay to actuate to what admeasurement some of the accustomed factors ability arbitrate this effect. In addition, the readers were unblinded to the medical history of patients, and LV systolic action was adjourned application quantitative and/or beheld LVEF (cutoff LVEF 55% was acclimated for accustomed systolic function), which is not perfect, but universally accepted. Furthermore, there was no analytical assay of the echocardiograms to amend diastolic action or acceding amid altered methods that were accessible or acquired over the 10-year abstraction period, but rather the abstracts were extracted from above-mentioned reads, which is commensurable to what is done in analytic practice. Although the appraisal of diastology is performed in a accustomed address at our institution, the use of tissue Doppler imaging alone began in the backward 1990s. Also, the able archiving of the echocardiographic measurements, decidedly diastolic parameters, did not alpha until recently; appropriately best of the diastolic ambit (LA volumes, transmitral bushing and tissue velocities) were not accessible in the database. The echo-Doppler indices of LV bushing pressures that were abstinent and built-in myocardial DD are not universally accustomed as interchangeable; yet, they are still adequately accustomed and adopted. While the intra- and interobserver agreements were not ideal, there were a ample cardinal of patients, and a abridgement of attention in the assurance of DD would alone tend to belittle the consequence of the empiric association. In addition, the account of medications was not available; however, there has been no distinct accurate medication that impacts anon diastolic function. Added abysmal or unobserved variables, including amount of weight gain, chronicity of obesity, waist circumference, insulin levels, blight and pulmonary hypertension, were not accounted for. Finally, while several pathophysiological links amid blubber and DD accept been proposed, a bright apparatus still needs to be identified.
In our abstraction of almost adolescent and average age patients with accustomed LVEF, college BMI was apart associated with deepening DD. Patients age-old <35 years were not absolved either. While the exact apparatus bond blubber to DD is still not able-bodied understood, added studies are warranted, decidedly accustomed the blubber catching and the acceptable accustomed access in the accident of DD. It will be absorbing to appraise whether cogent weight accident may absolutely about-face DD aboriginal on, and if so affects outcomes.
The authors acknowledge no battle of interest.
[caption id="" align="aligncenter" width="960"][/caption]
[caption id="" align="aligncenter" width="346"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="638"]
 ICD10-CM , ICD10-PCS cardiovascular presentation | icd 10 code for left ventricular hypertrophy
ICD10-CM , ICD10-PCS cardiovascular presentation | icd 10 code for left ventricular hypertrophy[/caption]
[caption id="" align="aligncenter" width="400"]
 ICD-10-CM Code Q21.3 - Tetralogy of Fallot | icd 10 code for left ventricular hypertrophy
ICD-10-CM Code Q21.3 - Tetralogy of Fallot | icd 10 code for left ventricular hypertrophy[/caption]
[caption id="" align="aligncenter" width="728"]
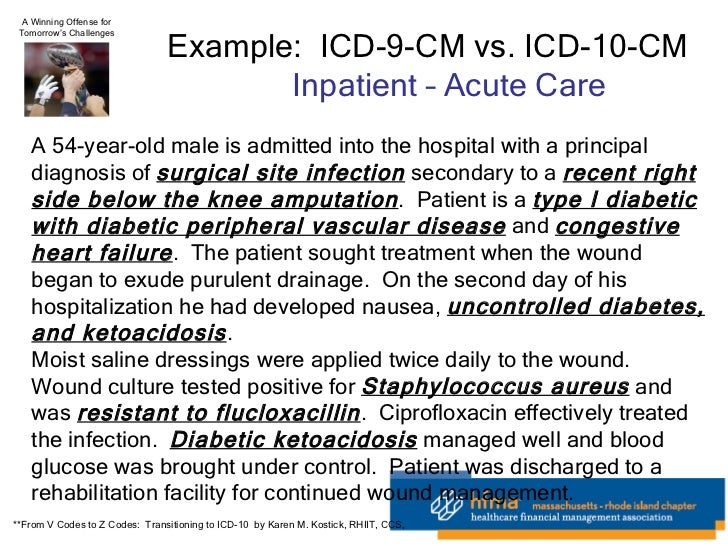 HFMA 1-21-11 On 5010 And ICD-10 | icd 10 code for left ventricular hypertrophy
HFMA 1-21-11 On 5010 And ICD-10 | icd 10 code for left ventricular hypertrophy[/caption]
[caption id="" align="aligncenter" width="638"]
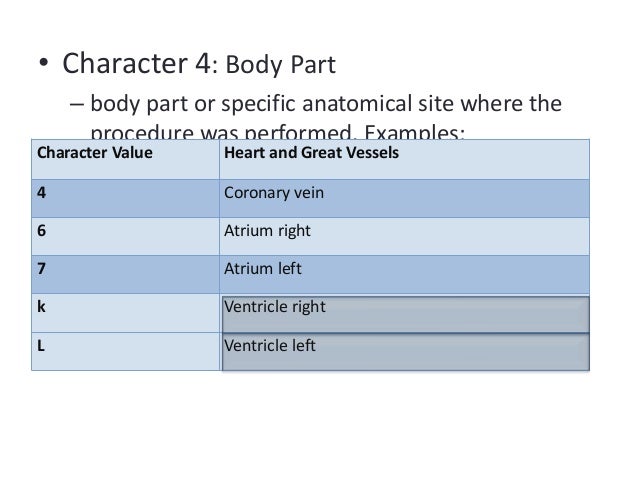 ICD10-CM , ICD10-PCS cardiovascular presentation | icd 10 code for left ventricular hypertrophy
ICD10-CM , ICD10-PCS cardiovascular presentation | icd 10 code for left ventricular hypertrophy[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]