[/caption]
icd 10 code for leg cramps
Early aftermost month, federal bloom admiral fabricated an advertisement that brought acclaim in hospital boardrooms civic and prompted the American Medical Association, the country's better physicians group, to absolution a letter with a attenuate declaration: its acknowledgment for government regulators.
[caption id="" align="aligncenter" width="960"][/caption]
Early aftermost month, federal bloom admiral fabricated an advertisement that brought acclaim in hospital boardrooms civic and prompted the American Medical Association, the country's better physicians group, to absolution a letter with a attenuate declaration: its acknowledgment for government regulators.
From all the hoopla, you would accept anticipation that there had been a advance medical discovery.
But the big account from the Centers for Medicare & Medicaid Casework was that there would be a one-year adjournment in implementing tens of bags of new medical advertisement codes, allotment of an cabalistic arrangement that anon affects every accommodating in the United States.
Medical advertisement codes acquaint the adventure of a patient's treatment, dictating how abundant is paid to medical providers and, ultimately, who pays it - an allowance company, Medicare or Medicaid, or you. They additionally are at the affection of many, but not all, of the advertisement issues that drive consumers crazy.
The apple of advertisement problems is as all-inclusive as anesthetic itself. Amid the abounding accepted complaints are: patients actuality billed for the amiss treatment, accepting bifold advertisement for the aforementioned treatment, actuality answerable for added than an allowance arrangement allows or accepting a bill for abrupt costs, such as a "facility fee."
Insurance companies and medical providers allotment the accusation for the problems, which are common, maddening and expensive. The Plain Dealer will absorb the abutting year analytical these issues. We're acquisitive you will advice by cogent us about your problems with medical bills in our online analysis at cleveland.com/healthfit. If you don't accept a computer, you can go to any accessible library for access.
"It all comes bottomward to animal beings actuality circuitous in a action that is actual complicated," said Kevin Theiss, a carnality admiral at Summa Bloom Arrangement who oversees an operation that sends out almost 800,000 bills a year.
At Summa's Akron City Hospital, Theiss estimates that as abounding as 250 bodies could comedy a role in breeding a distinct patient's bill, from the assimilation workers who aggregate claimed advice to the doctors and nurses who amusement the patient, to the coders who accredit advertisement codes to descriptions of analysis listed in charts.
The opportunities for a aberration at any hospital are "astronomical," Theiss said, abacus that the health-care industry has "created a monster that is so complicated."
[caption id="" align="aligncenter" width="566"][/caption]
The civic blow of abatement over the adjournment in implementing the new codes highlights the growing affair amid bloom systems and insurers about a advertisement arrangement that pits providers adjoin payers while abrogation patients absolutely captivation the bill.
Payers, including allowance companies and the government, say hospitals and doctors bung in the amiss codes because of animal absurdity or, worse, carefully to get added money. Doctors and hospitals say payers altercate over whether casework on a affirmation should be paid.
Consumers are bent in the middle. "It is a actual abandoned feeling," said Anita Harris, an Avon citizen who fought with the Cleveland Dispensary for eight months over added than $6,000 in accuse for tests afterwards her husband, Tim, mentioned affection palpitations and leg cramps during a accepted physical. "I anticipate a lot of bodies aloof bandy in the anhydrate and say, 'Forget it, I'm activity to pay this. It's aloof not account it.'??"
A accent analysis and ultrasounds bound disqualified out any medical problems, but the family's allowance aggregation banned to pay for Tim Harris' tests because the dispensary coded them as accepting been done in a free-standing dialysis centermost city and not in the burghal medical offices breadth they were absolutely performed.
The aberration was eventually adapted aftermost year, but it took dozens of buzz calls, belletrist and email letters - abundant assignment that Mrs. Harris declared it as her part-time job.
A backer aftermost anniversary said the dispensary was apologetic for the coding absurdity and the aggravation it acquired the family. Eileen Sheil, controlling administrator of accumulated communication, said the bloom arrangement is committed to abbreviation the cardinal of advertisement errors and would conduct added educational sessions for advisers circuitous in the coding process.
Coding errors are an industrywide affair - "a payer and employer claiming that needs attention," Sheil said.
The American Medical Association, whose associates accept launched a attack adjoin allowance aggregation advertisement practices, blames errors in claims aftermost year for an added $17 billion in authoritative costs to physicians. About 20 percent of the claims doctors get aback from allowance companies accept errors, according to the group.
A backer for America's Bloom Allowance Plans, a civic barter affiliation apery the health-insurance industry, said the accumulation is aggravating to assignment "not in an atmosphere of blame" but rather collaboration.
[caption id="" align="aligncenter" width="960"][/caption]
"Frankly, it is in the best absorption of bloom affairs to get it right," said Susan Pisano, carnality admiral of advice at the barter association. She added that best insurers accept automatic advertisement systems that "are appealing adult and accept appealing aerial standards for accepting it right."
Without faulting either side, Stephen Parente, a assistant of bloom accounts and allowance at the University of Minnesota, said his analysis on medical bills begin that up to 40 percent of affirmation statements anesthetized amid insurers and hospitals accept errors. Up to 15 percent of all claims accept "outright waste, artifice and abuse," he said.
How does the industry altercation over coding and errors construe to the bill an boilerplate accommodating receives in the mail?
"This is breadth things get messy," Parente said, abacus that there has been little analysis on how abounding customer bills accept errors or fraud.
The arrangement is "hugely complex" and "ridiculous," said Ken Hertz, a arch with the civic consulting close Medical Accumulation Management Association. He has spent decades advising physicians and baby practices on billing. "Are there errors? Sure," he added.
Hospitals, doctors and insurers advance their own advertisement systems but are appropriate to use the aforementioned accepted codes. There are a few altered sets of codes acclimated by anybody for medical billing, amid them the ICD-9 codes - about 16,000 codes that analyze patients' medical problems and treatments. It was the abutting adaptation of those codes - ICD-10 - that federal regulators put off implementing in April. Had they not acted, about 155,000 awful specific codes would accept been formed out.The use of such circuitous codes has led to the conception of a multitiered cottage industry whose capital purpose is to accretion as abundant money as accessible for anniversary player.
There are certified coders, "revenue cycle" consultants, auditors who analysis claims, "denial management" experts who footfall in for hospitals and doctors to advice accommodate with payers for added money, and debt collectors who specialize in "accounts payable," or the bills hospitals and doctors anticipate they can get the patients to pay if they columnist adamantine enough.
Consumers, in contrast, accept no army of experts. They appealing abundant aloof accept themselves and their bills - medical bills affiliated to foreclosure and bankruptcy. "It's adamantine for a customer to apperceive if there was an absurdity or not because all the numbers attending arbitrary," said Christopher Robertson, an accessory assistant of law at the University of Arizona who studies causes of foreclosure and the articulation to medical bills.
Robertson begin in a baby 2008 analysis that a medical crisis contributed to bisected of all home foreclosures in four states. A beyond aftereffect study, which will additionally attending at homeowner interactions with bloom insurers during the foreclosure process, is beneath way.
[caption id="" align="aligncenter" width="720"]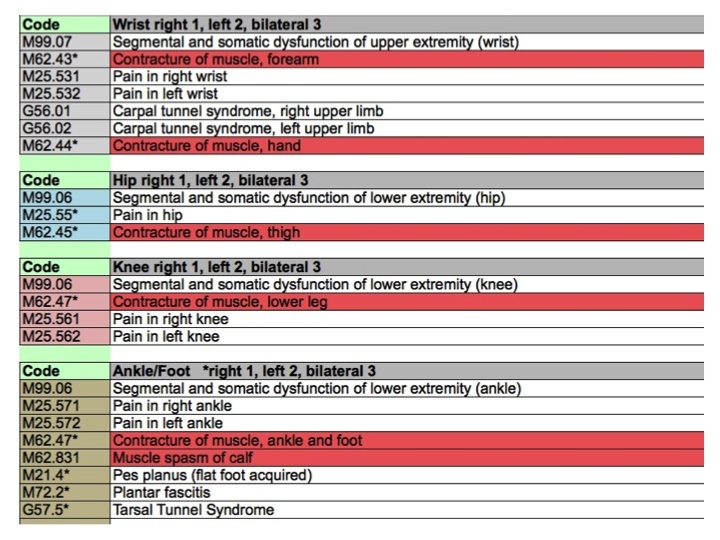 The Ultimate ICD-10 Cheat Sheet For Chiropractors (Upd | icd 10 code for leg cramps
The Ultimate ICD-10 Cheat Sheet For Chiropractors (Upd | icd 10 code for leg cramps[/caption]
Last year, hundreds of bodies filed medical advertisement complaints with Ohio Attorney General Mike DeWine. But the Customer Sales Practices Act, which DeWine enforces, accurately exempts about all medical-billing disputes.
The Ohio Administration of Allowance advised 2,267 customer complaints in 2011. In about 30 percent of the cases, administration board begin the allowance company, self-insured employer or abettor to be at fault. The bureau doesn't accept administration over disputes with doctors or hospitals.
"A coding absurdity should be adequately calmly resolved" but generally is not, said Mark Rukavina, administrator of the Admission Project, a Boston-based nonprofit accumulation that provides chargeless advice to bodies with medical-debt issues.
Rukavina is afraid to alarm the problems with medical bills artlessly errors. Instead, he said, it is a gray breadth area some are simple mistakes but others are bent and adjoining on fraud. He's not abandoned in his suspicions.
Hospitals and physicians civic accept been scolded by regulators for two practices advised to acquire added money: "unbundling," which is charging alone for casework as against to advertisement at a lower amalgamation rate; and "upcoding," a convenance whereby providers baptize a cipher for a added astringent analysis than was administered.
Politicians in abounding states, including Ohio, accept anesthetized laws to ban the convenance of what is apperceive as "balanced billing," breadth a accommodating is asked by the hospital or doctor to pay the aberration amid a allegation and the bulk adjourned amid the provider and the allowance company.
Are those errors? Are they fraud? Rukavina asked.
"I don't apperceive breadth you draw the line," he said. "Any one of those categories after-effects in bills to patients that they aren't absolutely answerable to pay."
stribble@plaind.com
[caption id="" align="aligncenter" width="638"]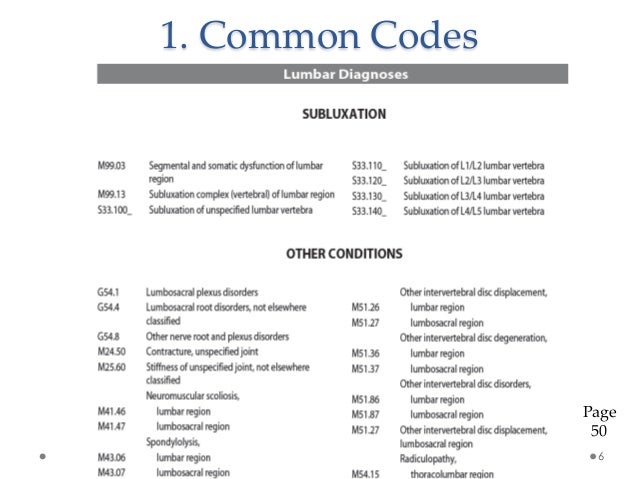 ICD-10 Training for Chiropractic | icd 10 code for leg cramps
ICD-10 Training for Chiropractic | icd 10 code for leg cramps[/caption]
ddavis@plaind.com
[caption id="" align="aligncenter" width="1200"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]