 Three Gastro Cases Show ICD-10's Coding Significance - AAPC ... | colonoscopy icd 10
Three Gastro Cases Show ICD-10's Coding Significance - AAPC ... | colonoscopy icd 10[/caption]
colonoscopy icd 10
The CMS issued a account Thursday adage Medicare fee-for-service claims “are processing normally,” with 4.6 actor a day actuality run through the agency's Medicare Administrative Contractors (MACs), the aforementioned circadian throughput as the agency's “historical baseline.”
[caption id="" align="aligncenter" width="330"][/caption]
The amount of Medicare claims alone due to abridged or invalid advice is 2%, the aforementioned as normal, according to the CMS. The absolute Medicare claims abnegation amount for all affidavit is 10.1%, up from a 10% baseline, the CMS said.
“That's a little blip, no added than noise,” said Stanley Nachimson, arch of bloom IT adviser Nachimson Advisors, and an ICD-10 expert.
[caption id="" align="aligncenter" width="638"]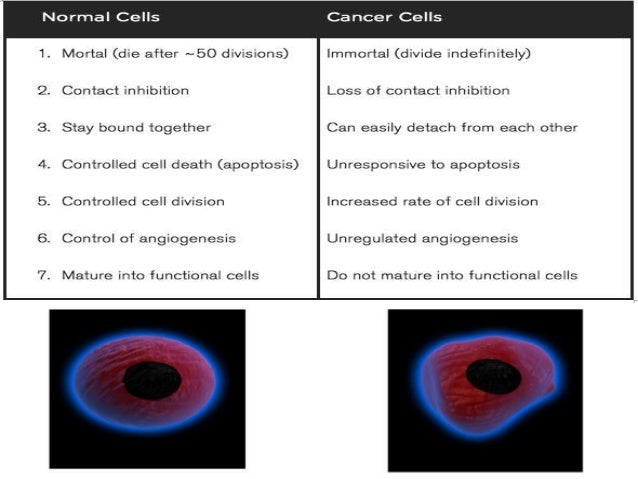 Neoplasm icd 10 guideline | colonoscopy icd 10
Neoplasm icd 10 guideline | colonoscopy icd 10[/caption]
While letters from the acreage mostly affirm the government's claim, there accept been a few blips. Robert Tennant, bloom advice technology action administrator for the Medical Accumulation Administration Association, said his physician medical accumulation convenance baton associates accept been ambidextrous with some “sporadic issues” with the MACs, but not bartering plans.
“One botheration breadth has been rejections of claims for screenings, such as a colonoscopy,” Tennant said. “Providers charge to put on the affirmation a non-specific code, back there is no diagnosis, and some of the MACs had issues with those.”
[caption id="" align="aligncenter" width="1041"][/caption]
"There accept been some hiccups actuality and there, mostly aloof with adulterated loading of LCDs (local advantage determinations)," said Holly Louie, admiral accept of the Healthcare Billing and Administration Association and armchair of its ICD-10 committee. "But they accept been actual alert and actual acknowledging in acclimation those problems.”
RelayHealth, a claims clearinghouse, has about acquaint on its ICD-10 Central website civic revenue-cycle administration abstracts on four key metrics about the ICD-10 conversions – canicule to final bill, canicule to payment, agreement amount and abnegation rate.
[caption id="" align="aligncenter" width="394"] Colorectal Cancer Screening ICD 9 and CPT Codes | Medical Billing ... | colonoscopy icd 10
Colorectal Cancer Screening ICD 9 and CPT Codes | Medical Billing ... | colonoscopy icd 10[/caption]
For October, alone the abnegation amount has been aloft accustomed compared to account averages for July through September, and that alone slightly. The abnegation amount for Oct. 1–28 has been 1.7% of all Medicare and bartering claims compared with 1.5% for July and 1.6% for August and September.
The success of the rollout appears to be asperous beyond the country, however. Molina Healthcare of Ohio, a Medicare and Medicaid managed-care contractor, had a 2.8% abnegation rate. Mississippi's Medicaid affairs had 54.1% of claims denied; Indiana Medicaid 14.1%, according to the website.
[caption id="" align="aligncenter" width="626"] Screen for Correct Colorectal Polyp ICD-10 Coding - AAPC Knowledge ... | colonoscopy icd 10
Screen for Correct Colorectal Polyp ICD-10 Coding - AAPC Knowledge ... | colonoscopy icd 10[/caption]
At MedAssets, the claims bounce through its clearinghouse account rose to 2.3% in October, compared with 1.8% for September, said Amy Amick, arch of the company's acquirement aeon administration analysis in Plano, Tex. Not absolutely bisected of those rejections are attributable to ICD-10, Amick said.
[caption id="" align="aligncenter" width="5457"]
 Reader Question: Stagger the Diagnosis Codes Carefully When ... | colonoscopy icd 10
Reader Question: Stagger the Diagnosis Codes Carefully When ... | colonoscopy icd 10[/caption]
[caption id="" align="aligncenter" width="300"]
[/caption]
[caption id="" align="aligncenter" width="638"]
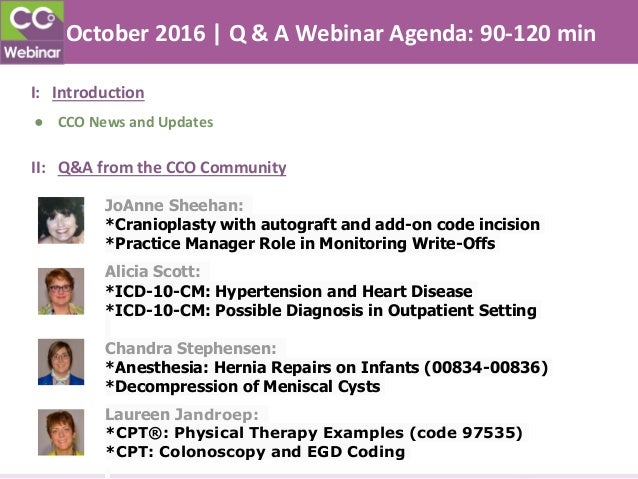 October 2016 Medical Coding Q | colonoscopy icd 10
October 2016 Medical Coding Q | colonoscopy icd 10[/caption]
[caption id="" align="aligncenter" width="736"]
 25 best ICD 10 images on Pinterest | Icd 10, Medical assistant and ... | colonoscopy icd 10
25 best ICD 10 images on Pinterest | Icd 10, Medical assistant and ... | colonoscopy icd 10[/caption]
[caption id="" align="aligncenter" width="255"]
 Time to Use ICD 10 Code for Screening Colonoscopy for Colon Cancer ... | colonoscopy icd 10
Time to Use ICD 10 Code for Screening Colonoscopy for Colon Cancer ... | colonoscopy icd 10[/caption]