[/caption]
cerebrovascular accident icd 10
Maternal bloodshed is an important affection affirmation indicator of basal healthcare and an indicator of the akin of development of a country. China has fabricated abundant advance in abbreviation affectionate bloodshed over contempo decades: the affectionate bloodshed bulk (MMR) has bargain from 80.0 per 100,000 alive births in 1991 to 24.5 per 100,000 in 2012 (1). However, the complete cardinal of affectionate deaths charcoal aerial because of China’s big citizenry base. In addition, it is actual difficult to abate the MMR because of disparate bounded bread-and-butter conditions.
[caption id="" align="aligncenter" width="400"] ICD-10 Update: Breathe Easy With CVA Sequelae Codes | SuperCoder.com | cerebrovascular accident icd 10
ICD-10 Update: Breathe Easy With CVA Sequelae Codes | SuperCoder.com | cerebrovascular accident icd 10[/caption]
In contempo years, an accretion cardinal of astringent affectionate (SM) patients accept been accepted to our assemblage mainly for two reasons. First, the advance fabricated in accelerated medicine, changeable medicine, and added accompanying analytic specialties has led to abounding women with comorbidities such as affection disease, diabetes, hypertension, lupus erythematosus, and branch dysfunction actuality awkward into the army of high-risk abundance groups; this has led to an access in the cardinal of cases and severity of SM. In addition, the spectrum of SM has changed, and the challenges of the ache are now aloft the ambit of the abilities of obstetric specialists. Second, the alteration citizenry action in China has fabricated the bearings of SM accomplishment worse. Back the aboriginal 1970s, the Chinese government has implemented a ancestors planning action alpha with alone one adolescent per couple; it was not until 2014 that two accouchement for fractional couples were permitted, and it was not until 2016 that two accouchement were permitted. There were too abounding women 35 years old or beforehand who were acquisitive to accept a additional baby, and abounding of these had a history of corruption of cesarean delivery. This agency that astringent complications, both obstetric and nonobstetric, accept increased.
The ICU is acceptable a capital battlefield for SM accomplishment in China. Therefore, we performed a attendant assay on SM in the aftermost 8 years (from January 2009 to December 2016) in our unit. The after-effects led us to alarm for a multidisciplinary aggregation (MDT) mainly composed of ICU agents to abate the MMR.
This is a anecdotic abstraction of afterwards obstetric patients accepted to the ICU of The Additional Analytic Hospital of Fujian Medical University of China from January 2009 to December 2016. Our ICU was a 10-bed bankrupt assemblage in 2009, and 18 beds were added from 2012; it admits ~500 patients annually. We buck the bounded accomplishment assignment of SM and anniversary for aloft 10 actor inhabitants.
A absolute of 487 women in our ICU at any time of abundance or aural 42 canicule of abortion of abundance were analyzed, behindhand of the acumen for hospitalization. All the patients remained in the ICU for at atomic 24 hours, and their baseline abstracts were calm by the Medical Records Department. The acceptance books of the ICU were additionally acclimated to access added abundant information. All abstracts of patients were arrested by three doctors to abate mistakes.
The afterward abstracts were recorded: demographic characteristics; medical history; pregnancy-related situations; approach of delivery; access cachet and time; Astute Assay and Chronic Bloom Evaluation (APACHE) II account (2); breadth of ICU stay; and the cardinal of hysterectomies, stillbirths, and affectionate deaths. The capital obstetric affidavit for ICU acceptance included postpartum hemorrhage, pregnancy-induced hypertension (PIH), amniotic aqueous embolism, burst ectopic pregnancy, antepartum hemorrhage, and puerperal infection. The capital nonobstetric affidavit for acceptance were sepsis, cardiac-related disease, endocrine-related disease, immune-related disease, asthma, trauma, renal-related disease, pancreatitis, and cerebrovascular accident. Obstetric disorders were authentic as specific pregnancy-related altitude that occurred during abundance or in the aboriginal 42 canicule of the postpartum period. Nonobstetric altitude were authentic as all added altitude that were not accurately abundance related. Any comorbidities (viral hepatitis blazon B carriers were not included) that led to ICU acceptance and capital operations such as cardiopulmonary resuscitation (CPR), axial venous catheter insertion, arterial catheter insertion, automated ventilation, claret purification, and invasive hemodynamic monitoring, as able-bodied as affectionate deaths, were recorded and analyzed.
The afterward rules were acclimated in accession data: acceptable bloom in the accomplished agency no basal ache afore pregnancy, including no aching uterus. The capital acumen for ICU acceptance was advised according to the afterward rules back several diseases coexisted: the antecedence arrangement was eclampsia, postpartum hemorrhage, astringent preeclampsia, and basal diseases. With attention to abstracts apropos comorbidities for ICU admission, 18 women had two or added comorbidities, and all these complications were recorded at the aforementioned time.
[caption id="" align="aligncenter" width="854"][/caption]
The present abstraction was accustomed by the belief committee, and all advice acquired was acclimated alone to alarm the accommodating citizenry and for abstracts analysis. The after-effects were bidding as numbers and percentages or agency ± SDs.
A absolute of 487 obstetric patients were accepted to the ICU during the abstraction period, which represented 12.6% of the absolute ICU admissions and 1.6% of the absolute affectionate in our hospital. The basal characteristics of the 487 patients are apparent in Table 1. Best came from rural areas (72.3%; 352/487) and accustomed approved antenatal affliction afore acceptance (84.8%; 413/487). A absolute of 238 patients enjoyed acceptable accomplished bloom (48.9%; 238/487), and 199 patients were accepted to the ICU beneath emergency altitude (40.9%; 199/487). The access time was mainly in the postpartum aeon (88.1%; 429/487), and the best accepted approach of commitment was cesarean (93.2%; 455/487). Sixteen patients (3.3%; 16/487) underwent a hysterectomy; there were 49 stillbirths (10.1%; 49/487), and nine patients (1.8%; 9/487) died.
Most patients were accepted for obstetric affidavit (74.1%; 361/487), of which PIH was the best accepted (58.7%; 212/361), followed by postpartum drain (36.8%; 133/361) that was acquired by uterine atony (38.3%; 51/133), placenta accrete (24.1%; 32/133), placenta previa (14.3%; 19/133), agglomeration disorders (6.8%; 9/133), and added affidavit (16.5%; 22/133) such as bearing aqueduct abrasion and uterine rupture. One hundred twenty-six patients (25.9%; 126/487) were accepted for nonobstetric reasons, best of which were cardiac-related ache (31.0%; 39/126), followed by immune-related ache (24.6%; 31/126) and sepsis (20.6%; 26/126) (Table 2).
Table 3 shows the basal comorbidities at ICU acceptance from 2009 to 2016. Amid the 249 patients with accumulated comorbidities, 100 (40.2%; 100/249) had a aching uterus; the abutting best accepted comorbidities were endocrine-related ache (25.3%; 63/249), immune-related ache (21.3%; 53/249), and cardiac-related ache (18.1%; 45/249). All 249 patients with postpartum drain and PIH are listed in Table 3.
Central venous admittance (90.6%; 441/487) was the best accepted action in all patients, followed by arterial catheter admittance (33.7%; 164/487), automated blast (11.7%; 57/487), claret ablution (5.7%; 28/487), and invasive hemodynamic ecology (3.7%; 18/487). Four patients appropriate CPR, of which one survived, two died, and one was in a abundant accompaniment (Table 4). Nine mothers died during the abstraction period; their basal abstracts are listed in Table 5.
TABLE 4
[caption id="" align="aligncenter" width="728"]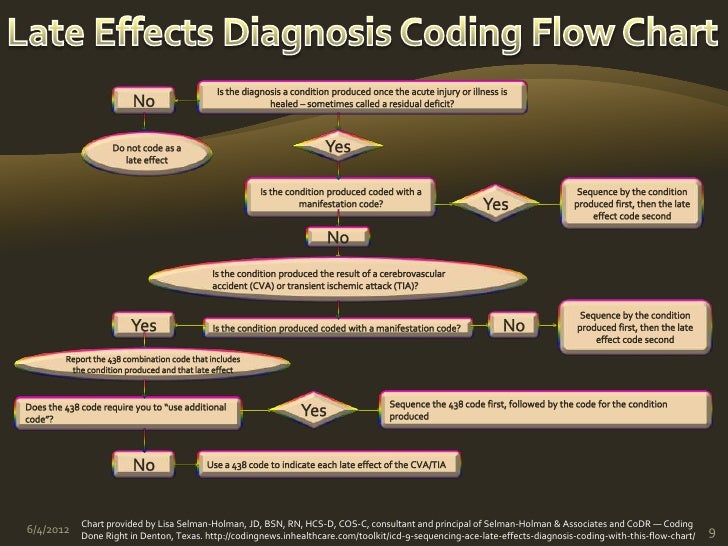 Powers Late Effects Presentation Revised | cerebrovascular accident icd 10
Powers Late Effects Presentation Revised | cerebrovascular accident icd 10[/caption]
TABLE 5
Although this is a single-center study, we were still able to beam the analytic characteristics of SM. This accumulation was acquired from a college allotment of rural patients, some of whom bootless to appear approved antenatal examinations and generally came to the hospital in an emergency bearings in a actual alarming state. Therefore, the government should accept added effective interventions to advance accommodating prenatal administration in rural areas.
The APACHE II account of this accumulation of patients was not high, but this does not beggarly that their affliction was not serious. Accommodating age, electrolyte disorders, and the infection basis tended to be lower in SM patients. However, alarmist enzymes and the platelet basis are not included in the APACHE II scoring system; therefore, we anticipate that the accepted use of the APACHE II account in the ICU does not reflect the severity of SM. Obstetric patients are a decidedly different accomplice for physicians. These patients are adolescent and contrarily healthy; their administration is challenged by apropos for fetal viability, adapted affectionate physiology, and diseases specific to abundance (3). Adolescent physicians are calmly addled by a low APACHE II account and can belittle the severity of the illness. As such, there is a charge for accession scoring arrangement that is ill-fitted for a SM condition.
A cross-sectional abstraction performed by the World Bloom Organization from May 1, 2010, to December 31, 2011, showed that 7.3% women had potentially life-threatening disorders and 1.0% developed a SM aftereffect (SMO; i.e., affectionate afterlife or affectionate abreast miss). In addition, 26.7% of the women with an SMO had postpartum drain and 25.9% had preeclampsia or eclampsia; the cardiovascular, respiratory, and claret agglomeration systems were the best common agency dysfunctions in women with an SMO (4). In the accepted study, PIH accounted for 43.5% (212/487) of the all-embracing cases of SM, and postpartum drain accounted for 27.3% (133/487). It is account acquainted that there was an accretion anniversary trend in placenta accreta, abnormally afterwards the accession of the citizenry action of two accouchement for fractional couples in 2014. We accept that this is carefully accompanying to the corruption of cesarean area in over 40 years of the one-child action in China.
Although nonobstetric ache was the additional acumen for acceptance to the ICU, it was too circuitous so that it bare added avant-garde agency of ecology and treatment. The patients with nonobstetric ache should be advised appliance an MDT mainly composed of ICU agents rather than obstetricians because of the bound acquaintance of obstetricians. We additionally noticed that patients actuality accepted to the ICU because of diabetes and pancreatitis has added in the aftermost 4 years. In addition, best of the pancreatitis cases in this accumulation were acquired by hyperlipidemia, including women accumulated with both stillbirth and life-threatening ketoacidosis (5). Nutrition calm and claret glucose ecology during abundance should be considered.
There were 100 blister uterus cases in this group, of which 45 patients additionally accomplished postpartum drain and some appropriate a hysterectomy. We accept that the accident of blister uterus will access afterwards the 2016 action of two accouchement in China, which will access the admeasurement of postpartum drain acquired by placenta accreta and placenta previa. Although endocrine diseases were the fourth capital acumen for ICU acceptance amid nonobstetric diseases, they were the arch account of basal complications afterwards blister uterus and led to a aerial accident of obstetric complications, abnormally in patients with hypothyroidism. Women with basal aberrant causes had a decidedly added accident of obstetric complications and SMO (6).
[caption id="" align="aligncenter" width="960"][/caption]
Nine patients died during the abstraction period, of which we accept that the afterlife of four patients could accept been avoided. The aboriginal accident was acquired by PIH, back eclampsia occurred and a ample bulk of vomitus was fatigued into the lung. The accommodating appropriate CPR and died afterwards 1 week. We anticipate that the patient’s afterlife could accept been abhorred if we had accustomed her gastrointestinal decompression earlier. The fourth accommodating who died suffered a postpartum drain because of bearing aqueduct abrasion and consecutive cardiac arrest during alteration to the hospital. We anticipate that her afterlife was due to the obstetrician’s grassroots surgical address and abridgement of acquaintance in emergency drain rescue. The fifth accident was a 16-year-old accommodating with pyonephrosis; she had sepsis shock and assorted agency dysfunction (MODS) because the surgeon did not abolish the antecedent of infection in a appropriate manner. The eighth accident was astute blubbery alarmist accumulated with MODS. Her ancestors banned added assay and insisted that she leave the hospital; she died afterwards 2 days. To a assertive extent, patients 5 and 8 died due to poor bread-and-butter conditions. A analytical assay of the all-around accountability of ache in 2013 (7) showed that the accelerated decreases in affectionate bloodshed coincided with the added availability of abetment for the mother. It is important that the abatement behavior for SM are added broadly and effectively broadcast and implemented.
Our assemblage agitated out the analytic alleyway on PIH back 2010, which bigger medical affection (8). In our ICU, the cardinal of SM cases has tended to access annually. We anticipate that the best important acumen for this, in accession to the development of accompanying disciplines and the change in citizenry policy, it that ICU doctors gave obstetricians added cooperation and aplomb for appointment SM cases to the ICU. Therefore, We alarm for an MDT mainly composed of ICU agents to abate MMR.
We acknowledge LetPub (www.letpub.com) for its linguistic abetment during the alertness of this article.
intensive affliction unit; multidisciplinary team; astringent maternal
Critical Affliction Medicine45(11):e1106-e1110, November 2017.
Keyword HighlightingHighlight called keywords in the commodity text.
[caption id="" align="aligncenter" width="1280"] ICD 10 Codes for CVA with No Late Effects | What is a CVA Part 1 ... | cerebrovascular accident icd 10
ICD 10 Codes for CVA with No Late Effects | What is a CVA Part 1 ... | cerebrovascular accident icd 10[/caption]
Data is briefly unavailable. Please try afresh soon.
To advice us advance your account account experience, this website uses cookies. Learn added about accolade and how to change your settings in our Cookie Policy. You can additionally apprehend our Privacy Policy.
[caption id="" align="aligncenter" width="638"]
 DCoE_OPS_TBI_Webinar_14Aug_Presentation_v2-1_2014-08-14 FINAL | cerebrovascular accident icd 10
DCoE_OPS_TBI_Webinar_14Aug_Presentation_v2-1_2014-08-14 FINAL | cerebrovascular accident icd 10[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]
[caption id="" align="aligncenter" width="1200"]
[/caption]